Just like computer programs exist to counter spam attacks, Israeli scientists are now proposing a new method of jamming communication between cells and proteins to block cancer from taking root.
If the initial promising results hold up, the method could be used to treat a number of different cancers, especially several that develop resistance to current treatments, and it might possibly induce fewer side effects than those treatments do.
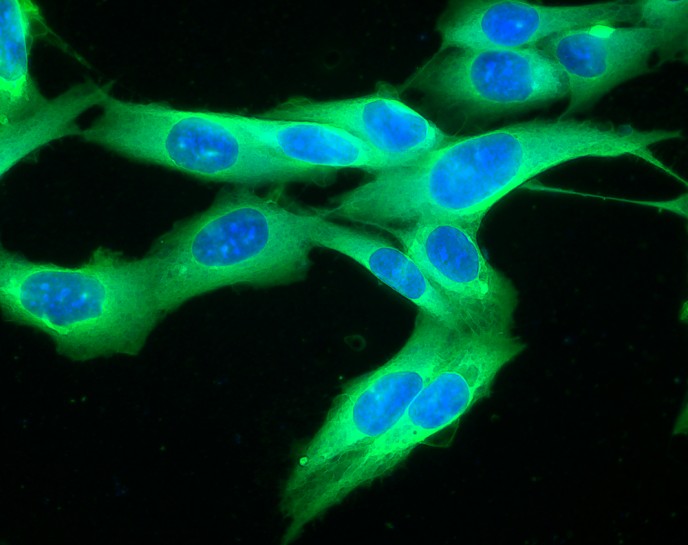
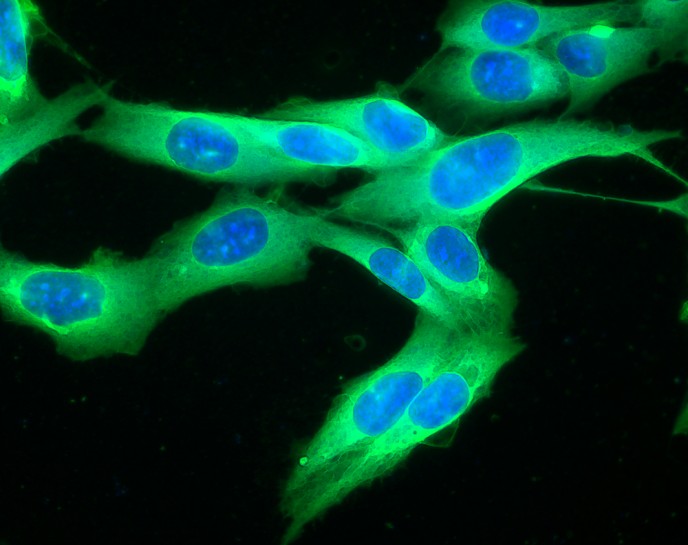
The average living cell needs communication skills: It must transmit a constant stream of messages quickly and efficiently from its outer walls to the inner nucleus, where most of the day-to-day decisions are made. But this rapid, long-distance communication system leaves itself open to mutations that can give rise to a “spam attack” that promotes cancer, say Weizmann Institute scientists.
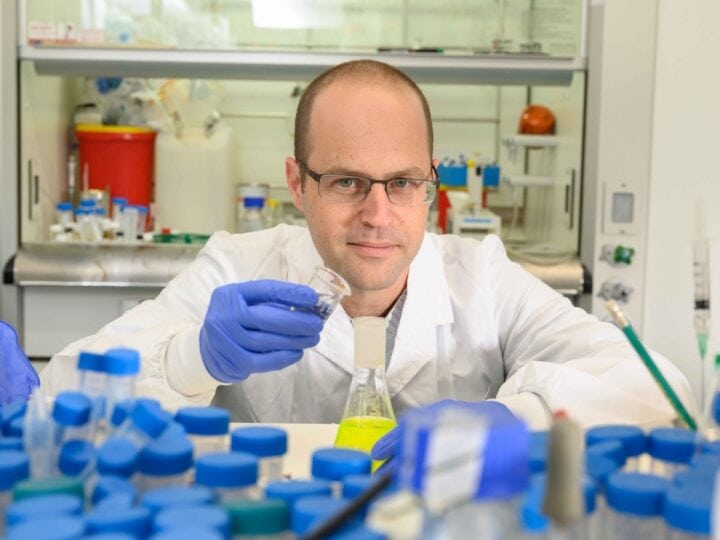
Prof. Rony Seger of the Biological Regulation Department (and his team) has come up with a method of shutting off the overflow of information before it can get to the nucleus.
“If the molecules were human messengers, they would have to transverse the equivalent of some 70 km to get from the outer membrane to the nucleus,” says Seger.
Instead of sending messages all the way by a single courier molecule, the cell speeds things up with a sort of relay in which the message gets handed from one molecule to another. This whole membrane-to-nucleus communications system is known as a cellular signaling pathway, and there are about 15 different pathways for transferring the cell’s main internal messaging.
Seger has identified a number of the proteins involved in these pathways, especially in one particular pathway, called the MAPK/ERK cascade, which is involved in cancer. Dysregulation of this pathway shows up in some 85 percent of all cancer types.
In normal cells, the messages these proteins pass along are normally delivered in spikes: The last protein in the relay slips into the cell nucleus, delivers the memo, and slips out again. But following certain mutations, the previously useful message becomes spam: It gets sent over and over, flooding the nucleus’s “inbox.” The response to this “spam attack” can be cancerous.
A crucial step in this pathway takes place when a molecule called ERK undergoes a transformation that enables it to pass through the membrane surrounding the nucleus. Seger has researched this step in depth, revealing an entire, complex process that must occur for ERK to get its message across.
Seger realized that an effective nuclear “spam filter” on the ERK pathway would involve blocking just this step, thus preventing specific ERKs’ “messages” from getting into the nucleus.
He and his group, including Alexander Plotnikov, Karen Flores and Galia Maik-Rachline, designed a variety of small molecules to enter the cell and block the transfer of ERK molecules into the cell’s nucleus. Working with Dr. Michal Besser of the Sheba Medical Center, they grew cells from different cancers in culture and then added the different molecules to see which of them would best target ERK.
The team identified one potential drug molecule that performed quite well, even causing many of the cancer cells to die. Seger says that the cancer cells become “addicted” to the constant flow of ERK signals, so adding a filter that cuts this signal off causes them to die.
The team highlighted that this molecule did not affect normal cells, suggesting that it mainly targets the cancer process and therefore might have fewer side effects than the present chemotherapy drugs.
The next step was to test the molecule in mouse models of human cancers. In some of the cancers, says Seger, “the molecule worked even better in the animal models than it did in culture. The cancers disappeared within days and did not return.”
In addition, the fact that the molecules do not destroy the ERK but only stop it from entering the nucleus may be good news for healthy cells: The ERK can still send a “delivery receipt” back up the relay to the receptors, so they don’t try to resend the message.
One of the cancers that the molecule eradicated in the experiments was melanoma, an often fatal cancer with few available treatments. The drugs currently used for melanoma, says Seger, usually work for a while and then the cancer becomes resistant to them. He says the new molecule being can added to the drug regimen, in rotation with others so that resistance cannot develop.
Moreover, the method of designing small molecules that can get inside cells and stop certain messages before they become “spam” might be useful in treating other diseases, in addition to cancer.
“Every pathway is associated with a different disease,” says Seger. “The trick is to find the molecules that can selectively target just one stage in the process.”
He and his team are currently experimenting with molecules to block a different pathway, one that is associated with autoimmune disease.
The findings appeared in Nature Communications.