There is no cure for Crohn’s disease or ulcerative colitis, the two chronic inflammatory bowel diseases (IBD) that cause flareups of abdominal pain, diarrhea, fatigue, weight loss and even malnutrition.
Ulcerative colitis affects only the colon, while Crohn’s can attack any part of the digestive system.
Although scientists debate whether IBD is an autoimmune disorder, they agree that the painful inflammation is caused by an abnormal immune response to lifestyle triggers (such as diet) and environmental triggers (such as bacteria).
While western Europeans and Americans are more commonly affected — roughly 300 of every 100,000 people – the incidence of IBD is growing in recently industrialized countries in Asia, Africa and South America.
There’s often a genetic component, too. Ashkenazi Jews are one of the populations at higher risk, and therefore IBD has become a research priority in Israel.
Current treatments include antibiotics, steroids and biological treatments aimed at inhibiting the activity of the immune system. These have long-term side effects, and do not get at the root causes.
Below are some recent research highlights that give hope to people suffering with IBD.
-
Viruses may vanquish IBD

An international team of researchers led by Prof. Eran Elinav of the Weizmann Institute of Science found a “silver bullet” approach to killing gut bacteria associated with IBD: common viruses called bacteriophages that selectively wipe out harmful bacteria in the gut microbiome.
After identifying the exact bacterial strains that play a role in human intestinal inflammation and implanting these bacteria into mice, the researchers screened thousands of phages and formulated a five-phage cocktail that significantly reduced intestinal inflammation and tissue damage in the mice.
In a follow-up trial with 18 healthy human volunteers, the phage cocktail was well-tolerated and didn’t cause negative side effects. Now it will be tested for safety and efficacy in larger clinical trials.
-
AI for early diagnosis
Diagnosing Crohn’s disease isn’t easy because its symptoms could indicate a variety of medical conditions.
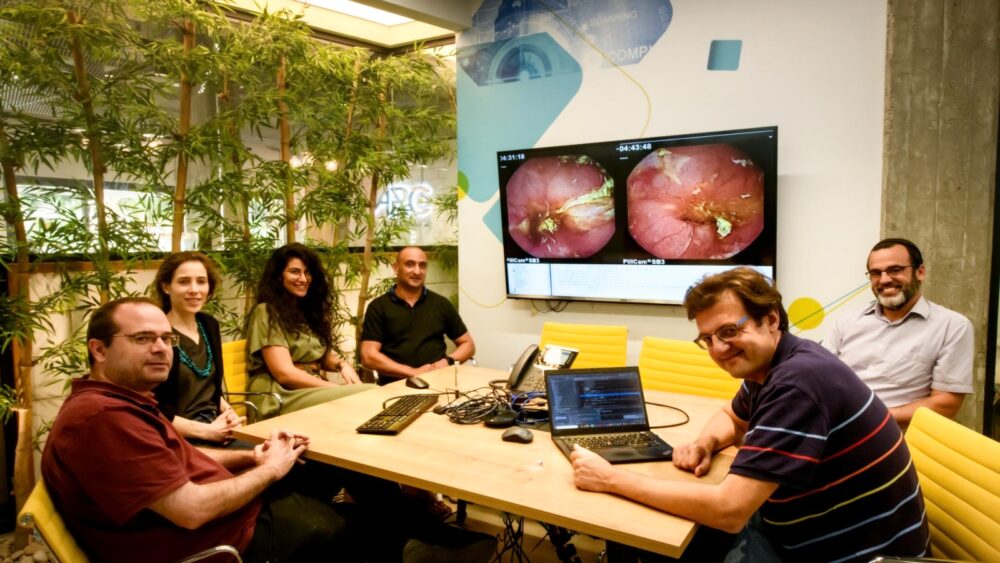
Now, an artificial intelligence-enhanced app developed by Intel and the ARC Innovation Center of Sheba Medical Center will help physicians diagnose Crohn’s at earlier stages and start treatment when it can be more helpful.
The app scans and analyzes up to 12,000 images taken by a “capsule pill” in the patient’s digestive system, with results in about two minutes.
In a clinical trial involving 101 patients, this method proved 86% accurate in image and data analysis compared to 68% accuracy achieved with analysis by an experienced gastroenterologist.
“Predicting the course of the disease in Crohn’s patients is one of the most important clinical challenges in the treatment of inflammatory bowel disease. However, currently available tools are limited and insufficiently accurate,” said Dr. Uri Kopylov, director of IBD in Sheba’s Gastro Institute.
The app will be available first at Sheba and later made available to other hospitals in Israel and abroad.
-
Ultrasound-aided diagnosis
Electrical engineering Prof. Yonina Eldar of the Weizmann Institute of Science and radiologist Ahuva Grubstein from Rabin Medical Center received a grant from the Israel Precision Medicine Partnership last year to develop a reliable early method for diagnosing and monitoring Crohn’s disease, as well as breast cancer, by visualizing the tiny new blood vessels they cause to grow.
In the case of Crohn’s, these new vessels grow in the bowel wall. But ultrasound images aren’t high enough resolution to show this change in microvasculature.
The scientists propose combining elements of artificial intelligence, physics and mathematics to make them visible. This would involve injecting and tracking the movement of microbubbles in the bloodstream to create high-resolution vascular maps.
In July 2020, the Israeli IBD Research Nucleus reported results of an observational longitudinal study of 156 adults with newly diagnosed Crohn’s disease from 2013 through 2017.
The goal was to see if it is possible to predict the course of disease in patients with a new diagnosis, which is a challenge because the early stages vary from patient to patient.
The researchers found that over the course of 17.2 months, 52 of the patients (33.3%) did not need interventions, while 29 (18.5%) required hospitalization and 75 (48%) were advised to start steroid, immunomodulator or biologic therapies.
They identified four factors that can be measured at diagnosis to identify patients at risk for a complicated course of disease: body mass index, serum level of vitamin B12, white blood cell count and serum level of ALT, a liver enzyme.
These guidelines could be used in patient management and selection of treatment.
-
Removing a cause of inflammation
Ben-Gurion University (BGU) of the Negev biochemistry and pharmacology Prof. Ehud Ohana found accumulations of succinate in the gut of people with IBD.
Succinate, a metabolic molecule involved in various biochemical cell processes, had previously been identified as a driver of chronic inflammation.
Putting those findings together, Ohana’s lab worked with colleagues in South Korea to formulate a novel treatment for IBD that removes the succinate accumulation from the body.
The university’s tech-transfer company, BGN Technologies, has filed for patent protection and now seeks a strategic partner for the further developing and commercializing this promising invention.
-
Kefir to the rescue

A different group of scientists at BGU found that molecules from the yogurt-like fermented dairy drink kefir can disrupt cell-to-cell communications in pathogenic bacteria, restoring balance to an overreactive immune system.
The molecules show promise for mitigating the extreme immune response in severe Covid-19 and could also tame acute IBD.
Following promising results in animal models, BGN Technologies is setting up a biopharma company for further development and clinical trials of the treatment made from kefir molecules.
-
Common link between Crohn’s and Parkinson’s
A study published in 2018 by an international group including scientists from the Hebrew University of Jerusalem and University of Haifa revealed a genetic mutation associated with a high risk of developing Crohn’s disease.
Surprisingly, the same mutation is known to increase the risk of Parkinson’s disease – a degenerative brain condition that, like IBD, is more prevalent among Ashkenazi Jews.
Regardless of what the connection may be, the researchers recommended that a relatively simple genetic test at a very young age could determine if someone carries this genetic mutation.
If so, medical monitoring and lifestyle choices – for example, avoiding highly processed foods and smoking — could make a difference in the progression and treatment of either disease.
In the longer term, the finding could lead to the development of a drug to lower the risk of developing either disease.
















