Professors Avigdor Scherz and Yoram Saloman of the Weizmann Institute in their lab – We see that the therapy results in the complete destruction of the blood vessels connected to the tumor.A revolutionary type of photodynamic therapy, developed in Israel, has shown great promise in treating men with prostate cancer – and could eventually be used to treat a myriad of other cancers as well.
Prostate cancer is the most common type of cancer found in American men, other than skin cancer. One man in six will get prostate cancer in his lifetime. The American Cancer Society estimates that there will be about 230,900 cases of prostate cancer in the US in 2004. Almost 30,000 men will die of the disease.
The new therapy is currently undergoing Phase II clinical trials in Canada, France, and Israel – with trials in the UK to start shortly. At three centers in Canada, the therapy – which employs a light-sensitive drug based on the plant pigment chlorophyll – is being used to treat patients who underwent unsuccessful radiation treatment for prostate cancer.
“The results are quite exciting,” said urologist Dr. Mostafa Elhilali, who is using the Israeli-invented drug, called WST09, to treat patients at the McGill University Hospital Centre (MUHC) in Montreal. “We have proof that this treatment causes the destruction of the part of the prostate which contains the cancer. We have patients whose blood tests show, after treatment, no cancer cells remaining. These are patients for whom radiation therapy failed,” noted Elhilali, who heads the Urology Department at MUHC and is also Secretary General of the International Urology Society (known by its French acronym SIU.)
Elhilali estimates that Phase III trials, to be held at multiple sites all over the United States and Canada, will begin some time in 2005. “We believe this treatment has great potential,” he told ISRAEL21c
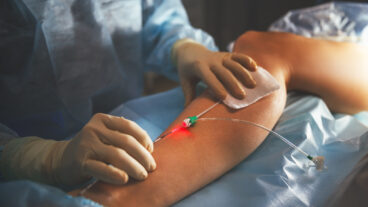
Photodynamic therapy (PDT) is a relatively new approach to treating cancer, which involves injecting a patient with special light-sensitive drugs. These drugs are harmless, until exposed to laser light whereupon they become toxic. Doctors can direct the light specifically to the site of the tumor, using optical fibers. This combination of light-sensitive drugs and light destroys the tumor cells, while leaving healthy tissue intact.
“It’s not a ‘shotgun’ approach, but rather a targeted approach,” explained Elhilali, “in which you cut off the blood supply to the tumor.”
The drawback of most forms of PDT to date is that they are effective only against relatively flat and thin tumors, such as certain types of skin and bladder cancers. In addition, the drug stays in the body for a long time, requiring patients to stay out of sunlight for lengthy periods following treatment.
However, the new drug, developed by scientists at Israel’s Weizmann Institute of Science – and now being clinically tested – has none of these drawbacks. It is based on chlorophyll, the green pigment that plants use for photosynthesis.
“Chlorophyll is designed by nature to harvest solar energy for photosynthesis, so it has high absorption of light,” explained Prof. Avigdor Scherz of the Weizmann Institute’s Plant Sciences Department, who together with Prof. Yoram Salomon of the Biological Regulation Department, invented the new photo-sensitive drug, WST09.
The chlorophyll pigment has the great advantage of being able to absorb near-infra-red light, which penetrates more deeply and efficiently than other wavelengths. The result: A single illuminated optical fiber can reach and eradicate a tumor with a diameter of up to 4 centimeters; larger tumors can be treated by using several fibers. This ability makes the treatment a suitable weapon against solid tumors that have, to date, evaded other photosensitive drugs.
In animal studies, other derivatives of chlorophyll, invented by the Weizmann group and developed by Steba Labs (Israel) and its parent company Steba Biotech (France), were able to destroy a variety of cancers, including breast, liver, kidney, colon, melanoma and glioma (a benign tumor of nerve tissue). “In our pre-clinical trials,” said Scherz, “we found that we were even able to target and eradicate metastases of prostate cancer in bones.
“In general, we see that the therapy results in the complete destruction of the blood vessels connected to the tumor, and necrosis of the entire tumor.”
Besides its potency, the advantage of the new drug is that it is flushed out of the body quickly – within hours, noted Scherz. “You don’t leave the patient with high sensitivity to light, which is one of the limitations of other photodynamic therapies.”
Unlike surgery, it is a non-invasive treatment with little risk and few side effects; therapy can even be repeated.
The Weizmann Institute scientists, together with Steba Labs, are now working to develop an array of chlorophyll-based drugs to treat various cancers. “We think that in five to seven years, we will have a whole arsenal of photodynamic drugs for treating different cancers,” said Scherz.
In the meantime, the first drug in this arsenal is showing promise in eradicating prostate cancer. It is now being tested in Canada, France and Israel, with advanced trials underway at Toronto’s Princess Margaret Hospital.
“I think photodynamic therapy is a revolutionary approach to the treatment of prostate cancer,” said Dr. John Trachtenberg, director of the Prostate Centre at Princess Margaret Hospital, who is conducting the trials in collaboration with Dr. Brian Wilson of the Ontario Cancer Institute. “So far we’ve seen prostate cancer eliminated with virtually no side effects,” Trachtenberg said recently. “This form of photodynamic therapy offers prostate patients an enormous opportunity for a second chance at a normal life.
“We’re very hopeful that we can not only use it to treat recurrent prostate cancer after radiation, but also to treat the primary disease, and you wouldn’t need radiation or surgery.”
“I truly believe this is the hope for the future and certainly hope for people with prostate cancer,” said Trachtenberg.
Adds Elhilali: “We are excited about this treatment because it means it could be a first line treatment comparable to successful surgery, but without the risk of surgery.”