We all want healthcare professionals to treat us as people, not numbers. To see us. Listen to us. Make medical decisions personalized to who we are.
But who we are is not just a matter of DNA, personality and life circumstances. We’re all generators of medical data.
Every checkup, blood test, drug prescription, therapeutic intervention, X-ray, ultrasound, MRI, CT, EKG, EEG, mammogram – you name it – adds to an unimaginable quantity of data that must be considered in delivering patient care.
The explosive growth of medical data, along with crisis-level personnel shortages and skyrocketing healthcare costs worldwide, points in one direction: artificial intelligence.

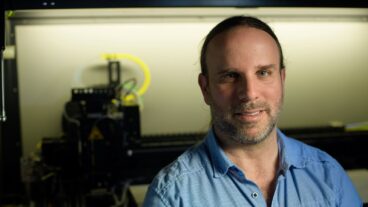
“Healthcare has huge challenges that we’ve not been able to solve using traditional means like adding more staff and buying more technology,” says Dr. Eyal Zimlichman, chief medical officer and chief innovation officer at Israel’s largest hospital, Sheba Medical Center, and founding director of its ARC Innovation Center.
“There are inherent challenges and barriers that require new solutions. AI can help us solve many of these problems,” Zimlichman tells ISRAEL21c.
“AI has the capability to considerably improve effectiveness and efficiency of healthcare systems by improving diagnosis and treatment decision-making for nurses and doctors based on large amounts of patient, imaging, clinical trial and evidence-based medical data that humans couldn’t possibly sort out,” says Zimlichman.
“When we’re able to treat precisely the first time, rather than the usual trial and error, we can avoid spending money on procedures and treatments that are not effective.”
Why Israel?
Israel, home to about 1,200 AI-related companies, is prominent globally in applying AI to healthcare among other verticals.
This is why the Carelon Digital Platforms subsidiary of Elevance Health, which insures 48 million Americans in 15 states, decided five years ago to establish its Global Tech Partnerships Hub in Tel Aviv.
“We’re using AI technologies from Israeli startups to create better whole care for our members, including behavioral and mental health,” says Udi Goori, general manager of the hub and its nearly 50 employees.

An AI-driven symptom checker from K Health has been integrated into Elevance Health’s mobile platform. Diagnostic Robotics is helping analyze members’ risk factors, enabling proactive patient engagement. TytoCare is using AI to identify which members should receive the TytoHome exam device and to analyze results.
Goori tells ISRAEL21c that the possibilities are vast, but “we need to go slowly and be very responsible in how we incorporate AI because we need 100% reliability of our solutions.”
Integrating AI technologies can be challenging, says Goori. “The lesson learned from the last few years is that it’s one thing to create and demonstrate something and another to develop, integrate and get it into the business responsibly,” he says.
“We have our center in Israel for that reason. We work on a daily basis with the startups in their own language and culture because it’s all about connection and integration.”
Below we’ll look at AI technologies already integrated into the healthcare systems in Israel and elsewhere, with more in development.
Image analysis

AI support of patient-care decisions using clinical image analysis is a growing part of the medical routine, says Dr. Leor Perl, head cardiac interventionalist and chief innovation officer at the innovation center of Beilinson Hospital in Petah Tikva, a 1,100-bed facility with a staff of 7,500.
Even experienced radiologists, cardiologists and oncologists can miss something tiny but potentially significant on a medical image, Perl tells ISRAEL21c.
“AI offers distinct advantages over people in quick computational ability with large amounts of data. For example, we cardiologists are very experienced in looking at EKGs but there are minute things we cannot see. AI can help us even to diagnose things we were not trying to see.”
Israeli AI is prominent in image analysis.
Aidoc is used in 1,200 hospitals – from the United States to the United Arab Emirates — to analyze imaging in emergency departments “where every minute counts, especially in stroke and other acute conditions,” says Zimlichman.
Aidoc has 13 FDA clearances and is analyzing a million patient images every month. Its rapid triage capabilities can shave an hour, on average, off an emergency room visit. Northwell Health, New York’s largest care provider, is now set to implement Aidoc in 17 hospitals.
MICA Medical uses AI to read mammography images and pinpoint tissue for biopsy.
“Right now we have a lot of false alerts where we have to biopsy something that turns out to be normal tissue,” says Zimlichman. “This is very stressful for the patient and we can avoid false alerts with more precise diagnostics.”
Nanox.ai (formerly Zebra Medical Vision) mines data from millions of existing medical images to highlight early, previously undetected signs of common chronic diseases. Its cardiac and bone solutions are FDA cleared, and its fatty liver solution is in development.
Sheba has introduced a new AI-powered cancer diagnostics research platform to accelerate the pathology department’s diagnostic capabilities. The first algorithm incorporated, developed by Imagene, identifies actionable biomarkers of non-small cell lung cancer from a digitized image of a conventionally stained pathology slide. Imagene reportedly shortens diagnostic time from three weeks to minutes.
Remote monitoring
Perl says that remote patient data collection became common during Covid “and we should do more of it. Not everyone has to come to a clinic or hospital for tests. Using AI, we can even adjust medications and detect emergent situations using remote sensing and monitoring.”
FeelBetter, which just raised $5.9 million and released retrospective research conducted at Brigham and Women’s Hospital in Boston, crunches clinical and pharmacy data to identify patients at high risk of preventable hospitalization due to poor medication management. The technology recommends precise interventions and follows the patient remotely to enable proactive and preventive care.
MyndYou’s active listening virtual care assistant, MyEleanor, engages at-risk patients in a personalized AI phone conversation about their health and lives. Using this data and detection of subtle voice changes, MyEleanor determines if follow-up is necessary and sends alerts, transcripts and actionable data to care teams.
One US client reported that 89% of discharged hospital patients engaged with MyEleanor in a 30-day wellness monitoring program that discovered 33% of patients were at risk of emergency room readmission.
Automating tasks
To ease a severe global healthcare workforce shortage, AI can automate tasks such as reading pathology slides and performing cardiology tests.
“We launched the company AISAP last year, which allows any doctor to perform echocardiography – an ultrasound test of the heart — that today has to be done by cardiologists. Sometimes patients need to wait a long time for an appointment, and in developing nations access is a problem,” says Zimlichman.
“AISAP also reads the scan and provides a full report, so it replaces both the technician and the cardiologist. Only patients identified with a pathological issue will be further examined by a cardiologist, minimizing their workload. We’re using it bedside in our general wards to make decisions on discharging patients faster,” says Zimlichman.
Navina, one of CB Insights’ Top 100 AI Startups for 2023, simplifies physician preparation for patient visits by creating an actionable “portrait” integrating patient data from electronic health records (EHR) and other sources.
Generative AI
Navina’s new AI assistant is the first generative AI tool purpose-built for primary care. It generates instant natural-language responses based on multiple sources including the patient’s EHR.
The goal is to streamline administrative tasks such as generating progress notes and referral documents, so that physicians can spend more time on patient care.
“Physician burnout from patient data overload has long been a critical issue in healthcare. Navina is committed to optimizing the technology that improves both the wellbeing and workflows of clinicians, and in turn, the lives of their patients,” said Ronen Lavi, Navina CEO and cofounder.
Kahun, which uses generative AI for medical decision support, recently launched a pilot integration in the triage process of the emergency room at Tel Aviv Sourasky Medical Center, Israel’s largest acute-care facility. Kahun’s chatbot provides pre-visit clinical insights about the patient’s symptoms, allowing the staff to focus on treatment and reducing fatigue and burnout.
“By standardizing these pre-visit assessments, we’re also eliminating bias and variability in care from the equation,” says Michal Tzuchman-Katz, cofounder and CEO of Kahun.
Generative AI for tasks such as summarizing recorded notes from patient encounters will have a growing role in reducing healthcare professionals’ workload and burnout, “letting doctors focus more on the patient than on typing into the computer,” says Zimlichman.
Eventually, he adds, “having a ChatGPT-type engine applied to clinical patient data in the future would allow us to get quick answers to complex questions.”
Legal, ethical implications
The potential capabilities of AI, and especially generative AI, raise some issues that even OpenAI founder Sam Altman has expressed concern about.
Beilinson Hospital, which recently created an introductory AI course for clinicians, hosted the Medical AI Roadmap Conference in January for Israeli doctors, academics, scientists and entrepreneurs to explore potential advantages and pitfalls of integrating AI into medical practice.
Should AI replace or augment physician performance? What are the legal and ethical implications of using AI and machine learning? How can AI-based healthcare maintain the essential aspect of empathy toward patients?
“Any tech that holds great potential comes with challenges and requirements in terms of regulations,” says Beilinson’s Perl.
“AI has gotten a bad reputation for fear of artificial beings that would dominate the world and put us at risk. But the advantages are far greater than the risks. Advanced software will enable us to do so many things more efficiently and accurately than we are doing today,” he says.
“You do need legal and ethical guidelines — the data has to be secured to make sure patients are safe. But that isn’t a reason to fear the rise of AI.”
Perl predicts that AI will become an increasingly helpful companion to the medical team in deciding when and how to intervene.
“Again, it’s about crunching all the data that humans just cannot do. Using AI for that would be instrumental,” he says.
“The next phase would be robotics. There are already surgical robots, but they are not fully autonomous. In the future, robotic surgical arms will be smaller, less invasive, quicker, and not operated by a physician. It sounds threatening but it’s promising.”
As a recent World Economic Forum report puts it: “While AI will not be the solution by itself, the transformative power of collaboration, responsible application and scaling of successful experiments can unlock its full potential, leading to better healthcare outcomes and the improved wellbeing of individuals on a global scale.”