A new smart probe for image-guided surgery developed in Israel may dramatically improve postsurgical outcomes for cancer patients.
Many cancer patients die not from the primary malignant tumor, but rather the spread of lingering cancer cells to other parts of the body, known as metastasis. The so-called “smart probe” developed by a team of Tel Aviv University (TAU) researchers may be able to help surgeons pinpoint cancer cells more precisely, allowing them to guarantee the removal of more cancer cells than ever before.
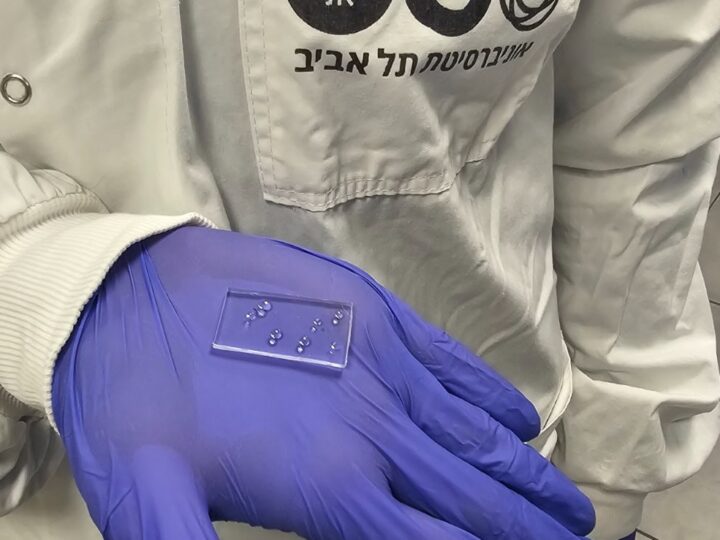
The smart probe, injected into the patient a few hours prior to surgery to excise the primary tumor, uses near-infrared technology to identify the cancer cells.
“The probe is a polymer that connects to a fluorescent tag by a linker. This linker is recognized by an enzyme called cathepsin that is overproduced in many cancer types,” says lead researcher Prof. Ronit Satchi-Fainaro of the physiology and pharmacology department at TAU’s Sackler Faculty of Medicine. “Cathepsin cleaves the tag from the polymer and turns on its fluorescence at a near-infrared light.”
The smart probes may potentially be used to guide the surgeon in real time during tumor excision. The surgeon can also avoid harming any “non-glowing” healthy tissue, the researchers said.
“In cases of melanoma and breast cancer, for example, the surgeon may believe he/she has gotten everything — that he/she has excised the entire tumor and left the remaining tissue free of cancer. Even if only a few cells linger after surgery, too few or too small to be detected by MRI or CT, recurrence and metastasis may occur,” Satchi-Fainaro said. “Our new technology can guide the surgeon to completely excise the cancer.”
Making cancer cells “glow in the dark”
As part of the study, the scientists first examined the effect of the probe in the lab on regular healthy skin and mammary tissue, and then on melanoma and breast cancer cells. Afterwards, they used mouse models of melanoma and breast cancer to perform routine tumor excision surgeries and smart probe-guided surgeries.
“The mice that underwent regular surgery experienced recurrence and metastasis much sooner and more often than those who underwent our smart probe-guided surgery,” said Satchi-Fainaro. “Most importantly, those which experienced the smart probe surgery survived much longer.”
The scientists are currently designing and developing additional unique polymeric Turn-ON probes for image-guided surgery, which can be activated by additional analytes such as reactive oxygen species (ROS), which are overproduced in cancer tissues, or by using other chemiluminescent probes.
“The probe may also reduce the need for repeated surgeries in patients with cancer cells that remain in the edges of removed tissue,” Satchi-Fainaro said. “Altogether, this may lead to the improvement of patient survival rates.”
The research team also included lab students Rachel Blau, Yana Epshtein and Evgeni Pisarevsky. They published their discovery in the journal Theranostics in June.
The research is based on long-term collaboration with Prof. Doron Shabat of TAU’s School of Chemistry, Prof. Galia Blum of the Hebrew University in Jerusalem, and clinicians Prof. Zvi Ram and Dr. Rachel Grossman of the department of neurosurgery at Tel Aviv Medical Center.
The research work done by the Satchi-Fainaro laboratory was supported by the European Research Council Consolidator Award, the Israeli National Nanotechnology Initiative, Focal Technology Area program, Nanomedicine for Personalized Theranostics, the Leona M. and Harry B. Helmsley Nanotechnology Research Fund, the Israel Science Foundation and the Israel Cancer Association.