As new superbugs become dangerously resistant to antibiotics, Israeli researchers have found a way to use the bugs’ mechanics to knock them dead.

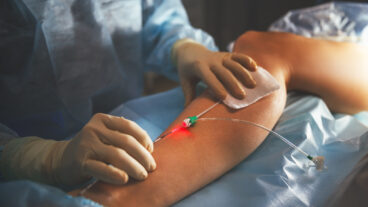
It’s the fight of the century: in one corner, the bacteria known as “superbugs,” and in the other corner the antibacterial drugs known as antibiotics. In bout after bout, newer and stronger superbugs are besting the antibiotics. And that alarms public health officials across the world, because drug-resistant bacteria cause infections – especially in already ill hospital patients — that are fatal 30 to 60 percent of the time.
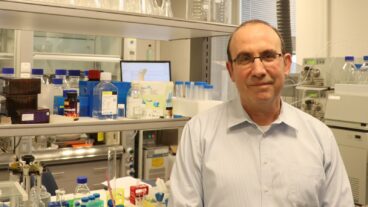
“Trying to keep pace with these ‘superbugs’ means always pulling out a new rabbit from the hat and using it for the next few years till there is another explosion of strains capable of overcoming it,” says Dr. Micha Fridman of Tel Aviv University’s Department of Chemistry. “This is a constant battle that I believe is never going to end.”
While scientists in Europe and North America continue the spiral of producing more powerful antibiotics to fight ever more powerful bacteria, Fridman and his University of Michigan research partner approached the problem from a different angle – one that uses the superbug’s own mechanics to develop antibiotics capable of delivering a decisive knockout punch.
Instead of looking for yet another “rabbit,” Fridman and Prof. Sylvie Garneau-Tsodikova and their research teams studied exactly how bacteria resist antibiotics. One method involves a protein or enzyme “machine” inside them that modifies the drugs.
Fridman explains this phenomenon to ISRAEL21C with the analogy of a key and keyhole. “There’s a keyhole in the door, and the door doesn’t want you to open it, so it somehow changes the keyhole and then you cannot push in the key,” he says.
As soon as a superbug’s “machine” recognizes the antibacterial “key,” it confounds the drug with a deactivating molecule. This additional molecule renders the antibiotic unable to reach its target.
The scientists described in the current issue of the journal ChemBioChem how they isolated the “machines” from superbugs. Then they chemically induced them to add a molecule that strengthens, rather than weakens, the antibiotic. Once an activating molecule is added, the superbug’s machine is incapable of adding a deactivating one.
In other words, Fridman and Garneau-Tsodikova found a way to beat the bacteria at its own game. Their lab-induced chemical alteration increases the antibacterial drug’s ability to fight bacteria and – most importantly — locks out the deactivating molecule that is the secret of the superbug’s winning strategy.

“Any sort of bacteria that uses this specific machine would not be able to deactivate antibiotics anymore,” Fridman tells ISRAEL21c.
Potential antibiotics enhanced by the duo’s discovery are a few years away from the market, since the full process of testing and government approvals is long and tedious – and only then can pharmaceutical companies begin mass-producing the drugs. But it is generating considerable interest, because the ability to beat bacterial resistance has become one of the holy grails in health care.
Other scientists are working on it, too. A three-year consortium of 14 European institutes was established in February 2009 to study the biology of drug-resistant bacteria and design novel strategies to kill them. And it was recently reported that a UK scientist has isolated a toxin from cockroaches that may hold promise in the superbug war.
In the meantime, hospitals worldwide are focusing more on prevention than treatment as existing antibiotics constantly lose effectiveness. Resistant bacteria have been reported by hospitals in at least 35 states of the United States, and cause deaths worldwide. In August, an outbreak at University College London Hospital killed one premature baby and sickened 12 others. Ironically, one of the most recent superbug battles took place right in Tel Aviv, where a hospital outbreak was traced to a patient visiting from New Jersey.
Tel Aviv is also where Fridman’s approach will soon be put to the test against many different problematic bacterial strains, at Ichilov Hospital-Sourasky Medical Center. This kind of study is tricky to carry out, said Fridman, because special equipment and procedures must be in place to safely deal with these dangerous superbugs.
The family of antibiotics his team chose to engineer is the one used commonly to treat respiratory infections in people with cystic fibrosis. “We do hope that some of the advances based on our methodologies can cope with this because it can be very lethal,” says Fridman.
He and Garneau-Tsodikova, who met at Harvard Medical School during their post-doctoral studies, financed their research with a two-year grant from BIRD, the Israel-US Binational Science Foundation and have applied for renewal.
“She sends students to me, I send students to her, and we are in touch through email and three times a week on Skype. We always write to each other about every single finding we have,” he says. They also visit periodically; Garneau-Tsodikova is due for a visit to Israel in January.