Professor Meir Bialer: For one third of epilepsy patients who are not seizure-free, we still need new anti-epilepsy drugsMost people think that epilepsy is under control; that it is an ‘old time’ disease which barely manifests itself anymore among the 2.5 million Americans who suffer from the neurological disorder.
But according to Professor Meir Bialer, the David H. Eisenberg Professor of Pharmacy at the Hebrew University School of Pharmacy, a pioneering epilepsy researcher, about one-third of the patients do not react positively to several existing drugs for epilepsy control on the market, and as a result, they continue to suffer periodic epileptic seizures.
“Most anti-epilepsy drugs are effective to a certain point. With existing medication, two thirds of patients are today seizure free. But one third are what we call therapy resistant,” Bialer told ISRAEL21c. “For this one third, we still need new anti-epilepsy drugs.”
Enter valrocemide, a drug developed by team lead by Bialer, who has authored over 180 publications in the area of pharmacokinetics, antiepileptics and central nervous system (CNS) drugs.
Following recent trials which demonstrated the efficacy of valrocemide as an antiepileptic drug, American drug company Shire Pharmaceuticals has signed a worldwide licensing arrangement for development, production and marketing of the drug with Yissum, the Hebrew University’s technology transfer company. Shire intends to study the drug as a candidate for application in a number of central nervous system conditions.
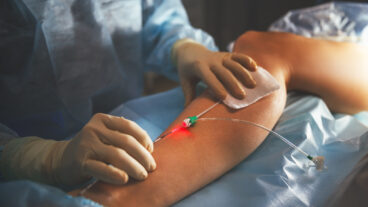
Epilepsy, a word of Greek origin meaning “to hold or seize,” is caused by brief bursts of electrical impulses in the brain. Seizures may be triggered by repetitive sounds, flashing lights, or touch to certain parts of the body, and can cause involuntary changes in body movement or function, sensation, awareness, or behavior. A seizure can last from a few seconds to status epilepticus, a continuous seizure that will not stop without intervention.
Seizures usually occur without warning and without the person’s awareness of what is happening. Some people with epilepsy will have only an occasional seizure, while others will have many on a daily basis. There are 125,000 newly diagnosed cases of epilepsy each year, and according to Bialer, the stigma attached to epileptic seizure go far beyond simple embarrassment or shame.
“If you have even one seizure a year, then in the US you’re excluded from getting a driver’s license. The social implications are huge – in American, without a driver’s license, you’re practically outside of society,” he said.
The ineffectiveness of current epilepsy medication for a third of the population stems from problems associated with glycine, an amino acid which epileptic patients have a shortage of. Glycine, like other amino acids in the brain, serves as a neurotransmitter, either excitatory or inhibitory neural transmissions within the central nervous system. Epilepsy is caused, among other reasons, by disturbances in the balance between these two functions: a rise in the level of the excitatory amino acids or a reduction in the level of the inhibitory acids.
Glycine is one of the inhibitory amino acids, and increasing its concentration in the brain has an antiepileptic effect. However, it is impossible to administer it to patients in its natural state, because it does not penetrate the blood-brain barrier that prevents medications from reaching their CNS target sites.
Bialer and his team, which included his former doctoral student, Dr. Salim Hadad, worked to develop a glycine derivative which would penetrate the blood-brain barrier.
The new CNS drug, valrocemide, is a combination of a known antiepileptic drug, valproic acid, and a glycine derivative, glycinamide.
“We combined chemically one of the major anti-epilepsy drugs with glycinamide, and managed to enable the drug’s permeability for brain penetration, enhancing it from 16 percent to 64%. And we’ve proven that it’s safer than other anti-epilepsy drugs which pregnant women and children are prohibited from taking,” said Bialer.
As he was preparing to leave to give a presentation at the Eighth Eilat Conference, a prestigious international gathering taking place this year in Spain which is focusing on anti-epileptic drugs, Bialer described his journey to becoming one of the top epilepsy researchers in the world.
“I’m a prickly pear through and through – a real Israeli sabra. I was born here, together with the state of Israel in 1948, a fact I’m proud of. I received my education from Hebrew University, and got my PhD there in medicinal chemistry, as well as an MBA. My mentor was Prof. Rafi Mechoulam.”
Mechoulam, a world renowned medicinal chemist and a pioneer in the field of cannabinoids who carried out his original cannabis laboratory experiments in the 1960s using contraband supplied by the Jerusalem police force, was the first scientist in the world to isolate THC – the active ingredient in cannabis. He also is credited with identifying the first endogenous cannabinoid.
“Mechoulam had told me stay out of medicinal chemistry as a career. I was sent to the University of Florida in Gainsville in 1977 to learn Pharmacokinetics – the study of what the body does to a drug. And when I came back, he gave me some more wise advice – find a field with scientific and academic independence. At his suggestion, I chose to specialize in anti-epileptic drugs, as well as other non-epilepsy central nervous system disorders. It was a suggestion I’ve strictly adhered to for the last 26 years,” Bialer said with a laugh.
The recent developments with velrocemide are part of Bialer’s efforts to see his research really aid the patients who need it.
“With any drug there’s a limit as to how much you can achieve in academia. Basically you can only move the tail of the mouse from the wrong side to the right side. At some point you need to get sponsorship if you want to really commercialize the drug,” he said.
Bialer was cautiously optimistic about the agreement with Shire and the further expected developments in testing velrocimide.
“We’ll be working together on the trials, but people shouldn’t be expecting to use the drug tomorrow, I don’t want to create any illusions I think the earliest we would complete Phase 3 trials and receive FDA approval would be 2011-12,” he said.
Besides valrocemide, Bialer, together with colleague Prof. Boris Yagan, have been busy developing other CNS drugs for epilepsy.
“We have three more lines of compounds that together with Yissum we’re in negotiations with American pharmaceutical companies for a licensing options,” he said.
The team was awarded a Kaye Prize for Innovation from Hebrew University this year for succeeding in developing a potential alternative for valproic acid (VPA), one of the leading antiepileptic drugs, which has been used as a central nervous system (CNS) treatment since 1967.
That drug also has serious safety drawbacks, with side effects that can cause damage especially to children or women of child-bearing potential. In their experimental search for an alternative to VPA, Professors Bialer and Yagen have developed propylisopropyl acetamide (PID), a new antiepileptic and CNS drug that has demonstrated excellent antiepileptic and antiallodynic (against neuropathic pain) activities, without the damaging side effects of VPA.
Bialer is non-committal when asked if he feels an affinity for one of his discoveries over another.
“It’s like having four children – You can’t ask which one is your favorite.”