For women struggling to conceive or maintain full-term pregnancies, the low success rates of assisted reproductive technology (ART) treatments (through which eggs are fertilized with sperm in a lab and then returned to a woman’s uterus)— only 20-30%, according to the Centers for Disease Control and Prevention (CDC) – are not always hopeful.
Now, a team of Tel Aviv University scientists say they’ve come up with a game-changing microscopic technology that will change the field of reproductive assistance.
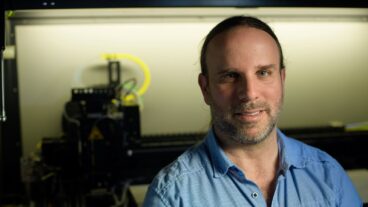
Dr. Natan Shaked, of the Department of Biomedical Engineering at TAU’s Faculty of Engineering, believes his new imaging process, which harnesses phase imaging methods to record the passage of light through a sperm sample to assess its thickness, can quantify the quality of sperm used in ART, leading to more successful ART treatments.
To date, there are two effective ART methods available: in vitro fertilization (IVF), in which a woman is treated with drugs that cause her ovaries to produce multiple eggs; and intracytoplasmic sperm injection (ICSI), in which a single sperm is injected into a mature egg and then transferred to a woman’s uterus.
Shaked’s method is applicable to both methods, but is especially helpful in ICSI.
“Until now, clinicians have chosen the ‘best’ sperm according to their speed, but speed is not necessarily an indicator of DNA quality,” says Shaked. “Some of the best sperm candidates are slow or even immobile because their tails have malfunctioned. If we can better determine the full structure and composition of the sperm, the success rate of ART treatments will be higher. Success means more births without congenital defects. In cases where sample staining is impossible — such as in vitro fertilization and ICSI — our device provides a promising new direction.”
Shaked’s new device, a small “black box” attached to an existing microscope, is smaller, cost-effective, and easier to align than conventional interferometric imaging methods. It is joined to new automated software that produces a thickness map of the sample and other physical parameters to evaluate the sperm’s viability in real time and, at a cost of only $1,000, can be used in any doctor’s office already outfitted with a conventional microscope.
Masters student, Dr. Miki Hifler, co-researched the study with Shaked. Sperm cells for the study were obtained from the Male Fertility Clinic at Chaim Sheba Medical Center in Israel. Findings were recently published in Fertility and Sterility.
The new method was developed with the support of Ramot, TAU’s technology transfer company The team recently submitted their patent on the technology and are poised to begin clinical trials next year on IVF patients in Israel.