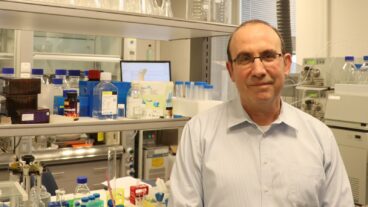
Prof. Shimon Efrat of the department of Human Genetics and Molecular Medicine at Tel Aviv University’s Sackler School of Medicine is hopeful that eventually human insulin-producing cells could be transplanted into human diabetics.The first steps to a cure for diabetes may have occurred, as investigators at Tel Aviv University announced the discovery of a new way to generate human insulin-producing cells in tissue culture. This ability has the potential to provide an abundant source of cells for transplant to juvenile diabetes sufferers.
The researchers, in conjunction with colleagues in the U.S., created insulin-producing cells from stem cells taken from the liver of a four-month-old miscarried human embryo and implanting them into Type I (insulin-dependent) diabetic mice. In this way, they managed to cure diabetes in mice.
Prof. Shimon Efrat of the department of Human Genetics and Molecular Medicine at TAU’s Sackler School of Medicine and colleagues in Israel and the US hope that eventually such cells could be transplanted into human diabetics – but only when a way is found to protect them from rejection through an autoimmune attack.
The important development – the first time that an unlimited supply of insulin-producing human cells has been developed – were reported in the Proceedings of the National Academy of Sciences.
In addition to Efrat and his colleagues at the Sackler School, other participants in the study included Drs. Sanjeev Gupta, Norman Fleischer and colleagues at the Albert Einstein College of Medicine in New York; and Dr. Mark Zern of the University of California at Davis Medical Center .
The genetically engineered human cells will theoretically be ready for clinical trials in two or three years, but in order it to become practical, some capsules or other “vehicle” that holds and protects the cells from being attacked by the body’s immune system must be developed. The team is working on such a vehicle, as are many other teams abroad, but so far no one has succeeded.
Efrat, who returned to Israel a few years ago after working at Yeshiva University’s Einstein College of Medicine, worked for 12 years on mice cells. Three years ago, the team advanced to human cells. The engineered cells produce about a third of the insulin made by insulin-producing cells in the pancreas. When transplanted into diabetic mice, the cells were able to reduce the elevated blood sugar levels and maintain a normal level for a period of several months. A third would be enough to cure Type I diabetes, which occurs when the body’s immune system mistaken recognizes beta cells as “strangers,” attacks them and destroys them. The body suddenly has no insulin to metabolize sugar in the blood, which can cause death without insulin injections.
“There have been suggestions of a synthetic structure to hold the insulin-producing cells while protecting them from an autoimmune attack, but it hasn’t yet proved itself. It’s likely that a combined technique will be developed,” Efrat told The Jerusalem Post. “If the cells become part of body tissue, with blood supply, it could be a one-time implantation, but if in a capsule, they would have to be implanted from time to time.”
Some 5 percent of the world suffers from diabetes, making it a major public health concern. Complications from diabetes include heart disease, strokes, kidney failure, blindness, and limb amputation. Type 1, juvenile diabetes, which is responsible for 10 percent of the cases, is caused by an auto-immune destruction of insulin-producing beta cells.
Type 2, adult onset diabetes, representing some 90 percent of the cases, afflicts mostly people aged 45 and older. It results from the body’s inability to respond to insulin, and is associated with obesity and a sedentary lifestyle, which explain its increased incidence in modern society.
In the U.S. treating diabetes costs about $100 billion a year, with the main treatment being insulin injections. But as the disease progresses, many patients need ever increasing amounts of the hormone, and the injection becomes less effective. The discovery of a more effective treatment cold significantly improve the quality of life of the patients.
The development is also expected to help patients with Type II diabetes, who produce some insulin but whose body suffers from insulin resistance, making its use inefficient. About a third of these patients have to inject themselves with synthetic insulin. If blood sugar levels are not kept in balance with insulin levels, the patient is at higher risk for a stroke, heart disease, blindness, and limb amputation.
Pancreas and islet transplantation have been severely limited by the shortage of donors and by the destruction of transplanted beta cells due to recurring autoimmunity. Efrat’s laboratory focuses on the development of new sources of beta cells for transplantation and on ways to protect them from immune attacks.
Beta cells do not multiply in tissue culture. In recent years investigators have attempted to generate beta cells from stem cells. Embryonic stem cells, derived from embryos a few days old, can replicate well in tissue culture and were shown to give rise to a variety of cell types. Fetal and embryonic tissues contain tissue stem cells, which are responsible for tissue maintenance throughout life. They too were recently shown to be capable of developing into other cell types.. Efrat is using genes known to play a role in pancreas development, as well as various inductive tissue culture conditions, to instruct stem cells to develop into insulin-producing cells in tissue culture.
“This work shows the potential of gene therapy for creating cells for transplantation,” said Gupta, a professor in the departments of medicine and pathology at Albert Einstein and one of the study’s authors. “We’re hopeful it will lead to insulin-producing cells being available on a large scale for treating children and adults with type 1 diabetes.”