The Israeli and Palestinian participants in the video conference.Psychiatrists and other mental-health professionals who treat devout Jews and Muslims have more in common than they imagine. Patients who think their mental illness is divine punishment for sins; their concern that if it became known, the stigma would hurt marriage prospects; and rituals considered by outsiders to be odd or obsessive are common to both communities.
British psychiatrists who until recently had no need to think about their patients’ religious practices now have to pay attention, given the massive influx of observant Muslims (with the accompanying distress caused by the dislocation of immigration) and the high birthrate of native Muslims. They also encounter haredi Jews, a growing sector in the British Jewish community.
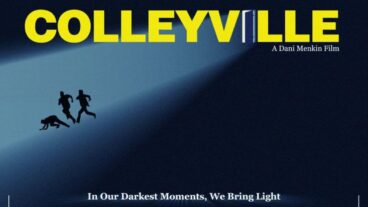
Israelis take Jewish and Muslim religious observances for granted, and there has even been research here on the interchange between religiosity and mental illness. Thus when two religious Jewish psychiatrists (one modern Orthodox and one haredi) and a Palestinian psychiatrist recently lectured to a British audience of mental-health professionals via videoconference from Jerusalem, the listeners were left open-mouthed. It was a new frontier.
The event was the first stage of an international debate called “The Interface Between Spirituality, Religion and Mental Health Services,” which linked Herzog Hospital in Jerusalem with University College London Medical School and Staffordshire University. The dozens of British participants, members of the multi-faith National Spirituality and Mental Health Forum – applauded enthusiastically and said they hoped more such broadcasts would follow.
The Israeli participants were Prof. David Greenberg, director of the Herzog Community Mental Health Center, who is an expert in the treatment of haredim, and Dr. Yakir Kaufman, the haredi director of Herzog’s neurological services. Dr. Bassam Al-Ashhab, a psychiatrist and professor at Al Quds University who directs community mental-health services in the Palestinian Authority, spoke about Islam and mental health after being introduced by Herzog director-general Dr. Yehezkel Caine.
Herzog Hospital, named for the late Sarah Herzog (wife of the late chief rabbi Yitzhak Isaac Halevy Herzog and mother of Israel’s sixth president, Chaim Herzog) was established in 1895 in Jerusalem’s Old City as a hostel for mentally ill people who were living on the streets. It became Israel’s first psychiatric hospital at the turn of the century, and in 1968 moved to its present site in Givat Shaul at the western entrance to Jerusalem. Due to the shortage of geriatric facilities in Israel, the hospital opened a geriatric division in 1977, which has since grown from 26 beds to over 200 of its 330 beds.
Caine noted that the hospital has a “true interfaith team,” and much experience treating haredim in its community clinic in northern Jerusalem that Greenberg directs. Greenberg, who also co-authored Sanity and Sanctity with Ben-Gurion University Prof. Eliezer Witztum, trained with Al-Ashhab in England three decades ago.
Greenberg explained to the British psychiatrists that the most important thing in the lives of haredim is keeping the laws of the Torah. “Therapists need to have an awareness of differences, and be willing to ask when they’re exposed to such a different community. We know our patients’ cultural and religious background. They regard contact with the outside world in general as corrupting, and the secular world in particular as problematic. They are very reluctant to seek help, as they see isolation as a virtue. In Israel, most psychiatric services are supplied by government, and few psychiatrists and psychologists are haredim.”
But, Greenberg added, “there are deeper problems. A devout Jew may say: ‘If I am suffering, presumably I have sinned. If I have sinned, why go to a psychiatrist?'”
Religious observances may even be regarded as pathological unless the therapist understands their origin, Greenberg noted. “If a haredi man is being treated by a woman, he will ask to leave the door open. This is because men and women who are not married to each other are not supposed to be in one place without a chaperone unless the room can be accessed easily by anyone. But the therapist will regard this behavior as strange and suspicious.”
A haredi man may be socially shy (which is perceived as a virtue), or may not look into her eyes or even at her. If he is given some bread to eat, he will pour water over each hand three times. This may look bizarre, but it is a normal ritual in this community.”
While there is apparently no higher prevalence of obsessive-compulsive disorder (OCD) among haredim than in the general population, when they do suffer from this condition it often presents itself as excessive ritual. “Invariably in men, OCD shows up as repeated and exaggerated praying, and washing themselves peri-anally before they pray. This behavior, we have found, is unique to observant Jews.”
Haredi women with OCD usually obsess about dietary and menstrual laws.
It is very important, Greenberg continued, to respect their social and religious hierarchy. It is very common for devout patients to come with a chaperone, and you have to accept it. Often, a patient will say he has to discuss a proposed treatment with his rabbi. Although this can be annoying, you have to accept it, as rehabilitation is a very value-laden concept.”
Stigma is a major deterrent in the community, mitigating against seeking treatment for mental illness, he explained. “Your marriage prospects and those of your relatives can be affected. When someone is considering a match, the potential spouse’s personal background and that of his or her family is investigated. Having to declare that you have psychological problems, even minor ones, and are taking medications can be a major disaster. Some haredi couples meet only once or twice before a decision to marry is taken, and merely revealing the existence of such problems can mean the end of a relationship.”
Someone in the British audience asked whether haredim with mental problems are able to get married. “Such a condition,” answered Greenberg, “means you’re not in the top league. If you have problems, you don’t get the best. If you have physical or mental illness, it’s harder, and you’re also more likely to marry somebody who also has a problem, such as a divorcée. It sounds like a marketplace, but this is the cultural context.”
He advises schizophrenics not to marry someone with the same disorder, because the risk would be higher for their children. “There are haredi matchmakers who specialize in ‘fixing up’ people with physical disabilities, but they aren’t interested in people with mental disorders. Nevertheless, many of my patients do marry.”
Al-Ashhab, who thanked the organizing committee for inviting him to speak, said that although he is a practicing psychiatrist, he hasn’t read much professional literature on the treatment of the devout. “However, I have much experience.”
Muslims pray five times a day, and view the Koran as a religious, not as a scientific book, he said. Al-Ashhab said Islam offers directions for living and dealing with day-to-day problems. “The concept of illness in Islam is that it comes by the will of God,” he said. “Emotional troubles are determined and written at the time of conception, according to Islam.” But the Koran also says there are other negative forces responsible for emotional distress and irrational behavior, including the Evil Eye (an envious glance thought to unintentionally cause illness) and jinn (a spirit that takes possession of a person and lives with him).
“Mental unrest is thought to be a manifestation of a heart and soul that is lost and distanced from its Creator,” the Palestinian psychiatrist explained. OCD can manifest itself in how many times a day you mention God. “It’s hard to persuade my patients that their mental illness hasn’t come from sinning.” Patients often go to many doctors, and when the problem is not relieved, they may come to believe it isn’t a problem that can be treated with therapy or medication.” Epilepsy is described by the Koran as being caused by a jinn entering the blood, causing convulsions, so patients go to a “religious healer.” More than 90% of Muslims with emotional problems consult religious healers before or after they see a psychiatrist, he added, and there are about 7,000 of them in the West Bank and 10,000 in Gaza. But there is a low suicide rate among observant Muslims, he said, because the religion says people “do not own their bodies.”
Islam, he concluded, “can be used for healing mental disorders. Because they trust Allah, they turn to Him in time of need for guidance and to ask forgiveness. Muslims are ordered to have a positive outlook on life, and they shouldn’t complain. They should endure illness patiently, as they believe cures are a sign of forgiveness.” Kaufman, an American-born haredi psychiatrist and Herzog expert in behavioral neurology and psychoneuroimmunology (linking emotion, the immune system and the mind) welcomed the unusual cross-continental encounter as a way to “enhance health services and offer more humane care for observant patients.”
The immune system, endocrine system, brain and nervous system should be in balance, he said. “Any change in a man’s state of mind can affect other systems and affect health for good or bad. Using neuroimaging, we can map emotional and even spiritual aspects of emotional changes on the human brain. We can even see the effect of prayer and meditation,” said Kaufman. “Stress has a harmful effect on the body and raises the risk for almost every disease, as it causes the secretion of hormones that if excessive can lead to chronic disease… I see many people who retire from a career that gave them their main source of meaning, become depressed and then chronically ill. Reducing stress makes you feel more controlled, and if that is enhanced by meaning, you can probably bring about a better health outcome.”
A growing number of studies show that people who attend religious services weekly reduce their risk of death from disease, and more frequent attendance reduces it even more, said Kaufman. He noted that the largely haredi city of Bnei Brak is among the poorest in the country, but has one of the longest life expectancies, contrary to the link between poverty and short lives in the rest of the world.
“I did a study published in Neurology that showed higher levels of spirituality or religious practices significantly slows cognitive decline in Alzheimer’s patients. If groups could learn Torah, pray and give charity together, I believe it could enhance spiritual well-being and even prevent pre-Alzheimer’s or slow a patient’s decline.” Can therapists representing the two religions create universal humanity? “We who give care like to have contact with other kinds of people, and find it pleasant to be together,” Greenberg concluded, “but we prefer to live with our cultural group. It is pleasant sitting together with such different world views, but we possess a common humanity.”
The Israeli, Palestinian and British participants agreed that psychiatric treatment is more effective when therapists fully understand the cultural and religious background and precepts of devout patients, and said they hoped the online dialogue would continue.