A neural network developed at the Technion – Israel Institute of Technology managed to correctly determine whether a breast cancer tumor expresses a protein that can be used for immunotherapy purposes – and where artificial intelligence disagreed with a human pathologist’s conclusion, a second test proved AI to be correct.
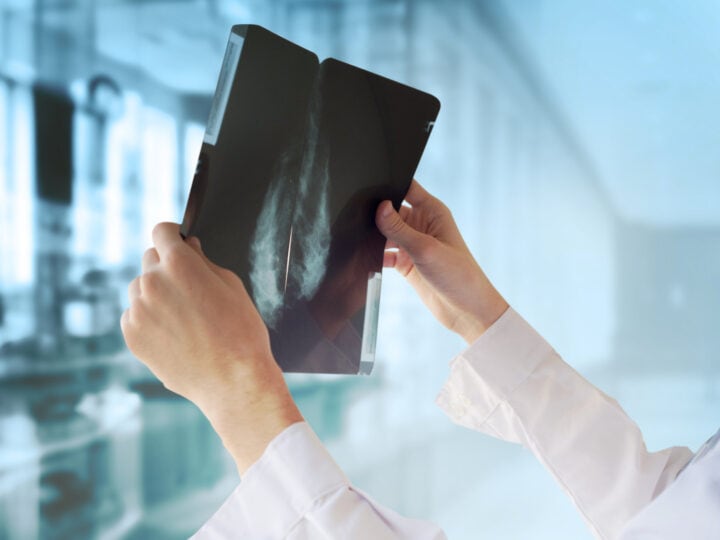
One in nine women in the developed world will be diagnosed with breast cancer at some point in her life, with the prevalence growing due to factors such as an increased lifespan and modern lifestyles.
And while personalized immunotherapy treatment is on the rise, the number of pathologists, or doctors who specialize in examining tissue to determine the specific diagnosis needed for personalized medicine, is on the decline.
This is where the Technion researchers stepped in, seeking to utilize AI to simplify and improve doctors’ work in a study that was recently published in the journal Nature Communications.
Sometimes, cancerous tumors exploit natural mechanisms that prevent our immune system from attacking our own bodies to evade it. One such mechanism sometimes displayed by tumors is related to the protein PD-L1, which acts as a sort of password that convinces the immune system not to attack.
To combat the tumor in such cases, specific immunotherapy for PD-L1 can persuade the body to ignore this password. But how do pathologists determine that the tumor expresses this protein? Traditionally, expensive chemical markers are used to stain a biopsy of the tumor, in a process that is both time-consuming at somewhat inconsistent.
The researchers decided to utilize already existing biopsy scans for diagnosis. They trained neural networks by presenting them with digital biopsy images from 3,376 patients that were tagged as either expressing or not expressing PD-L1. Then, the neural network was asked to determine whether additional clinical trial biopsy images from 275 patients were positive or negative for PD-L1.
The results turned out better than the researchers expected – in 70 percent of the patients, it correctly determined the answer, while in the other 30 percent it couldn’t find the visual patterns required for a decision. Furthermore, in cases where AI disagreed with a pathologist’s determination, a second test proved it to be correct.
“This is a momentous achievement,” explains Technion computer scientist Prof. Ron Kimmel. “The variations that the computer found – they are not distinguishable to the human eye. Cells arrange themselves differently if they present PD-L1 or not, but the differences are so small that even a trained pathologist can’t confidently identify them. Now our neural network can.”
“We expect AI to become a powerful tool in doctors’ hands,” he added. “AI can assist in making or verifying a diagnosis, it can help match the treatment to the individual patient, it can offer a prognosis. I do not think it can, or should, replace the human doctor. But it can make some elements of doctors’ work simpler, faster, and more precise.”