Omrix’s Omr-IgG-am is based on WNV antibodies derived from Israeli donors who have high levels of these antibodies.Mario Gamez, a 39-year-old electrician in Phoenix, recently spent six days in the Barrow Neurological Institute, part of St. Joseph’s Hospital and Medical Center, with a case West Nile encephalitis.
The father of three boys received another experimental treatment, a form of interferon, but several weeks into his illness, Gamez is still too exhausted to work and is coping with weight loss and partial paralysis of his face.
But soon, through a collaboration between the National Institutes of Health and an Israeli biotech company Omrix, hospitals throughout the United States – including Barrow – are set to begin expanded testing of a unique Israeli blood treatment for patients with extreme cases of West Nile Virus.
The West Nile virus infection in humans is making a big comeback in the United States this summer, with the pace of this year’s epidemic expected to surpass last year’s. So far this season, 265 cases of the disease have been identified in 18 states, up from the same time last year, according to the Centers for Disease Control and Prevention in Atlanta, Georgia,
Arizona is home to the largest number of cases, according to recent federal figures.
As of last week, the state has reported 161 cases, almost half of the total of human cases in the United States this year and more than 10 times the number it reported last year. In California, state officials there have reported 42 human cases to the CDC so far this year, a jump from a total of three last season. They’ve also attributed the state’s first death to West Nile.
Until recently, human infection with West Nile virus, which is spread by mosquitoes, was limited to Africa, Asia and the Middle East. Since its arrival in the New York City area in 1999, human WNV infection has increased in scope and severity in the United States each year. In 2003, the U.S. Centers for Disease Control and Prevention reported more than 9,860 cases of WNV disease, which included 264 deaths.
But hope is in the offing with the NIH trials which involve a drug that includes human plasma from Israeli donors The multi-center trial, which opened at 36 sites last September, is expected to add about 24 new sites this summer throughout the United States and Canada, pending internal approval at each institution.
The Phase I/II study is a safety trial to determine whether immunoglobulins, or antibodies, in blood from Israel, where the mosquito-borne virus is endemic, can lessen the disease’s severity in patients with West Nile encephalitis or those at risk of developing the brain-swelling complication.
“As West Nile virus disease continues to spread across our country, it is critical that we develop specific treatments for its most severe symptoms,” says Anthony S. Fauci, M.D., director of The National Institute of Allergy and Infectious Diseases. “At present, clinicians have few options besides supportive care for treating people with WNV illness. By expanding this study, we hope to accelerate NIAID’s efforts to understand, develop treatments for and eventually prevent this disease.”
Israeli company Omrix is providing its product, Omr-IgG-am, for use in the trial. West Nile virus has circulated in Israel for decades, and many Israeli blood donors have antibodies to the virus. The company’s product is based on WNV antibodies derived from Israeli donors who have high levels of these antibodies.
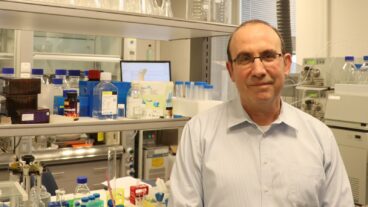
“The great bird migration between Africa and Europe goes through the Jordan Valley in Israel, and the birds spread mosquitoes who carry the virus through the route. Although we’ve had isolated cases over the last 10 to 20 years, there wasn’t much attention paid, and gradually Israeli plasma has grown naturally immunized to the virus. This isn’t the case in American or European plasma,” Omrix director-general Nissim Mashiach told ISRAEL21c. “That’s one of the reasons the NIH has decided to test our product.”
The trial can enroll up to 110 patients 18 years old and older who have WNV-related encephalitis or are who at risk of developing this severe neurological complication. Participants will receive a single dose of Omr-IgG-am or a dose of one of two placebos.
Patients with flacid paralysis, Parkinson’s-like tremors and those who slip into comas also are eligible to receive the Israeli product, which contains antibodies to fight the disease. In Arizona, the Mayo Clinic Scottsdale, Barrow Neurological Institute in Phoenix and the Arizona Health Sciences Center in Tucson were expected to participate in the safety trial, pending approval. The Indiana University School of Medicine became involved with the study in September but so far has not enrolled any participants.
There is no approved treatment for people who contract West Nile virus, which is spread by mosquitoes that feed on infected birds and then bite humans. The majority of those infected will have no symptoms, but about 20 percent will develop West Nile fever, meningitis or encephalitis.
Those who are sick enough to be hospitalized typically receive “supportive care,” including pain medication, fever reducers and intravenous fluids. In the most serious cases, patients will be moved to an intensive-care unit, given a feeding tube and placed on a ventilator to assist in breathing.
In the NIH trial, patients will be infused with one dose of Omr-IgG-am within seven days of exhibiting symptoms of the disease. But because this is a double-blinded controlled scientific trial, some patients will receive a placebo, immunoglobulin taken from U.S. blood donors or saline. They will not be told which substance they are given, nor will their doctors know, and will be monitored.
Each patient will have a greater than 50 percent chance of getting the Israeli blood product, Walla Dempsey, who is overseeing the study as an NIH clinical trials program officer, told the Arizona Republic.
“When you have a new disease emerge, it’s difficult to know what’s going to work because many people get better on their own,” she added.
Omr-IgG-am is effective for six weeks. It is based on a protein group found in the blood’s liquid component called immunoglobulin, which is taken from blood donors found to contain active antibodies against the virus.
“This group contains all the antibodies that a human develops in his lifetime once he is exposed to bacteria, viruses and the like,” said the developer of the drug Professor Bracha Rager. Until recently she was chief scientist of the Health Ministry, and is also a veteran researcher at Ben-Gurion University of the Negev’s microbiology and immunology department. Her collaborator in the research was Dr. David Ben-Nathan of the Biological Institute in Ness Ziona.
The researchers succeeded in isolating the “defensive antibodies” produced from a group of proteins taken from Israeli blood donors who had come in contact with the virus. The antibodies were injected into mice who had been infected with the West Nile virus. The disease was eliminated in the intentionally infected lab mice, and it has already promoted the recovery of a woman at Netanya’s Laniado Hospital.
As a result of their work, published in the July 2003 issue of The Journal of Infectious Diseases, the collaboration was hatched between the NIH and Omrix, who licensed Rager’s technology and developed Omr-IgG-am.
In Israel, West Nile infections are common enough that a large percentage of residents are exposed in childhood, when they are likely to avoid serious illness but develop antibodies to the virus. Those antibodies provide the lifelong immunity.The Israeli immunoglobulin is manufactured from pooled donations of plasma, one component of blood, so it’s not necessary to test individual donors for antibodies.
That’s how immunoglobulin is made in the United States, too, but according to Indiana University’s Dr. Kenneth H. Fife in a statement to Indystar.com, it’s believed that not enough Americans have been infected with West Nile for antibodies to show up in immunoglobulin made in the United States.
Participants are being recruited through NIAID’s Collaborative Antiviral Study Group (CASG), headed by Richard Whitley, M.D., of the University of Alabama at Birmingham. Information about the trial is located both at CASG’s Web site.
Omrix’s Mashiach is hopeful that the final Phase III trial will soon follow the current trials, and that Omr-IgG-am will then receive FDA approval and be a forerunner in helping to prevent the spread of West Nile virus throughout the U.S.