As the head of the Anxiety and Stress Research Unit at Israel’s Beersheva Mental Health Center for the past decade, Dr. Hagit Cohen knows too well that there are currently no medications that directly address the core symptoms of post-traumatic stress disorder.
In recent years, reaction to extreme trauma has become an important area of research worldwide with much interest coming from the United States following the September 11 attacks. Now with American soldiers returning home from Afghanistan and Iraq with symptoms of post-traumatic stress disorder, new directions for dealing with it are receiving increasing international attention.
According to promising research conducted by Cohen and her team at Ben-Gurion University and recently published in the American Journal of Psychiatry, a treatment called Transcranial Magnetic Stimulation (TMS) may hold out some hope for an effective future therapy.
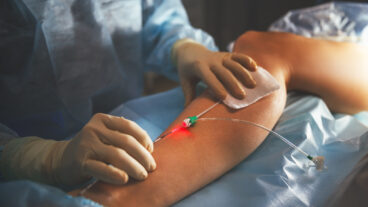
This use of magnets, Cohen explains, has been used for many years by neurologists for assessment purposes. For the past decade, the psychiatry field has been testing their use therapeutically, primarily among patients suffering from depression, as an alternative to electric shock therapies.
Unlike the use of electric shock, TMS does not require anesthesia and does not have problematic side effects. Using this noninvasive technique for directly stimulating cortical neurons. electrical energy can cross the brain almost painlessly, without causing convulsions or cognitive impairment.
Based on the therapy’s promise with depression treatment, Cohen and her team at BGU decided to explore its possible effectiveness with the many trauma victims they work with in their clinic who suffer from different types of post-traumatic stress disorder (PTSD).
“They range from those who have reactions to military combat, motorcycle accidents, work accidents, abuse, assault or unexpected death of a relative,” Cohen explains.
Events as varied as an earthquake, a war, sexual/physical/emotional abuse, a devastating fire, a rape, a stock market crash and accidents of all kinds can be the precipitating factors to the development of symptoms.
For some, the traumatic episode is relatively recent; for others, many years have passed. What they have in common is the core symptoms of PTSD – an overwhelming response to an extreme event or series of events. Merely experiencing the event itself does not qualify a person for a PTSD diagnosis – the symptoms following the event are the key.
Symptoms include the recurrent and intrusive distressing recollections of the event; recurrent nightmares of the event; intense psychological distress at exposure to internal or external triggers that symbolize or resemble an aspect of the trauma; avoidance of thoughts, feelings, or conversations associated with the event; avoidance of activities, places, or people that arouse recollections of the trauma; inability to recall an important aspect of the event; markedly diminished interest in important activities; a restricted range of feeling or estrangement from others; a sense of a foreshortened future; difficulty falling asleep or staying asleep; irritability or outbursts of anger; difficulty concentrating; hyper vigilance and an exaggerated startle response. According to Cohen, not all of the symptoms must be present; however, what symptoms there are must be connected to the trauma experienced.
The recent BGU research suggests that repeated stimulation of certain brain regions with magnets can help alleviate the debilitating PTSD symptoms. In an earlier study conducted by the team, two patients with PTSD had experienced improvements after treatment with magnetic stimulation.
In the recently published BGU study, the group evaluated the therapeutic effects of low- and high-frequency magnetic therapy as compared with fake therapy in 24 patients with PTSD recruited from the inpatient and outpatient treatment programs at Cohen’s clinic.
The patients were randomly divided into three groups: some received the high frequency magnetic stimulation, other will have low frequency magnetic stimulation, while others received therapy without the magnetic therapy (placebo). Treatment was administered during their daily 20-minute sessions during a 2-week period.
The stimulation was applied to the region of the brain called the prefrontal cortex, which has an “important role in mediating responses to stressful situations,” Cohen says.
Drug treatment was neither stopped nor changed in the three weeks prior to the study or during the study. Patients continued to receive the same individual and group supportive psychotherapy as before the intervention. The severity of PTSD, depression and anxiety were blindly assessed before, during, and after completion of the treatment protocol.
The team found that the magnet therapy had a positive effect, and specifically that patients experience more improvement with high-frequency therapy than low-frequency therapy or the placebo therapy. After their ten daily treatments, the high-frequency therapy patients experienced greater reductions in anxiety, greater feelings of comfort and slept better.
Generally the treatment was well tolerated and cooperation was excellent among all patients who completed the course and it had no effect on any patient?s blood pressure or heart rate during the treatments. No serious side effects as seizures, neurological complications, or cognitive difficulties occurred.
Cohen says that the results of this relatively small preliminary study means that continuing trials of high-frequency magnetic therapy with PTSD patients should be conducted.
She notes that while most pharmacological treatment improves the depressive and anxiety aspects of PTSD more than the core symptoms, the TMS therapy appeared to spark improvement in the PTSD core symptoms more directly than medication. This widens the scope and possibilities of the treatment efficacy of TMS.
But Cohen remains cautious. “It is still in the research phase, and preliminary, but what we have found gives us the green light to continue. It is a good beginning and points to a direction that is a promising avenue for the continuation of the research with PTSD patients.”