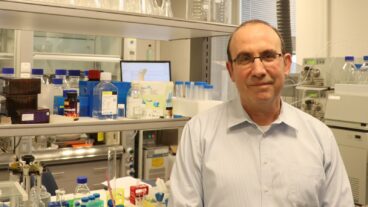
Professor Ariel Miller: This project will help prevent side effects, the resultant hospitalization, and will avoid giving medication which doesn’t fit. It will have a major economic impact.Imagine this scenario: a patient goes to visit his family doctor complaining of allergy systems. He takes his gene card out of his wallet and hands it to the physician, who swipes it through a runner connected to his computer. Immediately, all of the data about the patient’s genome – his genetic makeup – appears on the screen, and from that information, the doctor is able to prescribe the appropriate medication that will be most effective without causing any side effects.
A futuristic pipe dream? Not according to Professor Ariel Miller of the Technion’s Rappaport Faculty of Medicine and head of the Multiple Sclerosis and Brain Research Center at the Carmel Medical Center in Haifa, Israel. Miller is leading an ambitious consortium involving scientists and engineers from five Technion faculties, which is attempting to locate genes that will enable tailoring drug therapy to each patient individually. This could solve one of the most difficult problems currently facing physicians: which drug to prescribe to a patient and in what dosage.
“The current mode of most medical treatment is based on trial and error,” Miller told ISRAEL21c. “Let’s say a patient comes to a doctor and is diagnosed with hypertension. The physician prescribes a medication – but it’s basically a gamble as to whether that med is the best one for the patient. Then over the next few months, you see how the patient responds. If there’s not sufficient results, you might increase the dosage, and if there are side effects, you might switch the medication.
“So, the possible end result is that for a few months, the patient might suffer from side effects from a medication which is insufficient in the first place.”
The Technion gene project will solve that problem by pinpointing individualized medicine tailored to the patient in accordance with his genome. According to Miller, it will enable the attending physician to predict reaction to the drug treatment and will replace the ‘trial and error’ medical treatment used today.
“If a patient has a certain genome, he’ll react to medication differently than a person with another genome,” he succinctly explained.
Five faculties and ten scientists – from Medicine, Industrial Engineering and Management, Bio-Technology and Food Engineering, Bio-Medical Engineering and Computer Science – have joined together for project, including Technion faculty and physicians from Rambam, Carmel and Haemek Medical Centers, together with their assistants.
“The computer scientists among us will develop methods to analyze the genetic data and genomes that will be provided to them by the physicians and scientists,” explained Professor Ron Pinter, of the Technion’s Faculty of Computer Science, and an expert in bio-information who is coordinating the project with Miller.
“Ultimately, we hope to create the guidelines that will enable physicians to more effectively administer medication. The bottom line is that we’ll be able to provide the tools that will be able to tell which medication that’s available on the market will be the most effective for a given patient,” he told ISRAEL21c.
The project is being sponsored by the Wolfson Foundation of Great Britain and the Galil Center at the Technion, and was launched following the initial success of research that Miller and his team have conducted over the last four years related to pharmacogenetics – the science of tailoring medications according to an individual’s genome.
“Around four years ago, coinciding with the work on the Human Genome Project [the 13-year effort to identify more than 20,000 genes in the human DNA lineup], we decided to deal with the issue of how it can be used to physically change the way patients are treated,” said Miller.
A team of neurologists and scientists from the Technion – in collaboration with the Israeli Ministry of Industry and Trade and with the pharmaceutical company Teva – tried to answer a relatively simple question related to Teva’s groundbreaking drug for multiple sclerosis – Copaxone.
“The Multiple Sclerosis and Brain Research Center at the Carmel Medical Center were very involved in testing Copaxone, the world’s leading drug for treatment of MS – we were the first to discover how Copaxone worked in humans,” said Miller.
The question they attempted to answer was – when you have a new MS patient, how do you decide whether to give them Copaxone or something different?
“For every treatment, patients are categorized as ‘good responders’, ‘poor responders’ and ‘adverse responders’. We genotyped – or analyzed – hundreds of patients who have received Copaxone over the years, then compared their genetics. We looked for things like if there was a common denominator among all good responders, and likewise with the other responders,” Miller said.
“We’ve received positive preliminary results. We fished out a number of genes that possess crucial ‘SNPs’ [‘single nucleotide polymorphisms’ – which are DNA sequence variations that occur when a single nucleotide in the genome sequence is altered.] These genes define whether a patient will respond to a medication or not. Now we need a bigger, more advanced study which is why we’ve launched this expanded group under the headline ‘Personalized Medicine,'” added Miller.
Lack of information as to what drug is suitable for which patient and what dosage is needed, harms patients and creates unnecessary expenses arising from hospitalization as a result of drug reactions and even disability caused to patients, according to Miller.
“Going back to the hypertension example, if you misdiagnose for many months, it could result in the patient having a stroke, or myocardial infarction. This project will help prevent side effects, the resultant hospitalization, and will avoid giving medication which doesn’t fit. It will have a major economic impact, by lowering hospital stays and money spent on ineffective medication. We’re talking about millions of dollars,” said Miller.
Among the issues that the consortium will be investigating besides the continued MS research are – treatments for psoriasis – does a patient respond better to UV or to sunlight? And antibiotics – why certain people who get certain antibiotics suffer hearing loss. And, according to Miller, the issue of personalized medicine is not just for medication, but also for lifestyle.
“For example, we may map the genome for the kind of person who is prone to get a headache after drinking a glass of red wine.”
With five faculties and many researchers involved in the project, Miller and Pinter are optimistic that the varied skills and interests of the team will work together in harmony.
“Part of the problems are already behind us – we’ve agreed on a common agenda,” said Pinter, who has a masters and PhD from MIT and has worked for 20 years in industrial research and computation biology. “We’ve developed a good rapport among ourselves and have developed a common language. We’re enlisting our own toolboxes, skills and techniques to benefit whatever we know in the specific context of a problem.
“We’ve already taken the first steps by organizing four research teams to work together on specific issues. The first team to actually meet is looking at the issue of data integration – how to organize multitudes of data types, and how to get the most amount of information available. This will help us learn where we need to conduct more research and experiments,” Pinter said.
According to Miller and Pinter, the gene project highlights the unique ability of the Technion to integrate engineering, scientific and medical capabilities, one that is not surpassed in the world.
“I think we’re among the world’s leading teams in the field, and we’ve just received grants from the Wolfson Trust for the purchasing of cutting edge technology for genotyping, which will allow us to do a number of things we hadn’t been able to,” said Miller. “We have a unique environment at the Technion – a combination of top scientists, physicians and engineers. When I go to speak abroad, I say it’s like putting together Harvard and MIT,” he said.
Added Pinter, “the Technion is unique in that it’s a technical university with a medical school. There’s very few in the world. Here you have people with skills in engineering, math and computer sciences working side by side with researchers in medical science and with practicing physicians.”
In the future, Miller hope the project will lead to the development of new drugs according to the patient’s genome. But in the much more immediate future, there’s the gene card.
“The vision that the patients will come to the family physician with a disk on key – a ‘Health Key,’ or maybe it will be like a credit card. All the information of their genome will show on the computer, and the physician will be able to match it to the right medication.
“This is not so far off in the future. In some diseases, it’s already applicable. The FDA announced two years ago that only women with a certain genetic makeup would benefit from a certain medication for breast cancer. So now every woman with breast cancer who is recommended to take this medication is going through genetic studies.”
While coordinating the various faculties and individuals involved in the consortium is a daunting task, Miller is accepting it with good spirits, and a bulldog determination that focuses on the goal line. “In the future such a personal health card can save human lives.”