Cancer relapses are the worst. You’ve gone through invasive treatment, maybe surgery, hoping that will knock out the disease forever and then, boom, it’s back.
Israeli scientists now say they have managed to slash the incidence of breast cancer relapse by up to 88 percent by adding a second drug to chemotherapy.
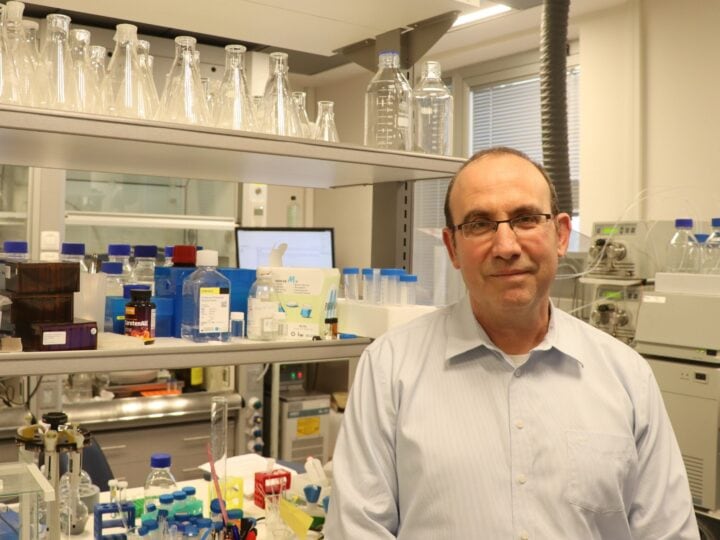
The catch: It only works in mice so far. Adapting the method for humans could take another five to 10 years, Prof. Neta Erez and her team at Tel Aviv University say.
Still, it’s a potentially major advancement that could revolutionize cancer treatment.
The peer-reviewed research was published in October in the scientific journal Nature Communications.
The problem, Erez explains, is that cancer cells can travel from the main tumor site and “hide” elsewhere in the body.
Erez speculates it may be the chemotherapy itself that’s enabling breast cancer cells to evade detection.
“Chemotherapy has some undesirable and even harmful side effects, including damage to healthy tissues,” Erez says. “The most dangerous of these is probably internal inflammations that might, paradoxically, help any remaining cancer cells to form metastases in distant organs. The goal of our study was to discover how this happens and try to find an effective solution.”
In the lungs
The most likely place for breast cancer cells to hide out is in the lungs.
“What we showed is that tissue damage induced by chemotherapy instigates an inflammatory response in the lungs,” Erez says. “Then, if small amounts of breast cancer cells are left in the lung, this inflammatory response triggered by chemotherapy ironically makes these cells thrive, and creates a hospitable environment for cells which then go on to cause a relapse of breast cancer.”
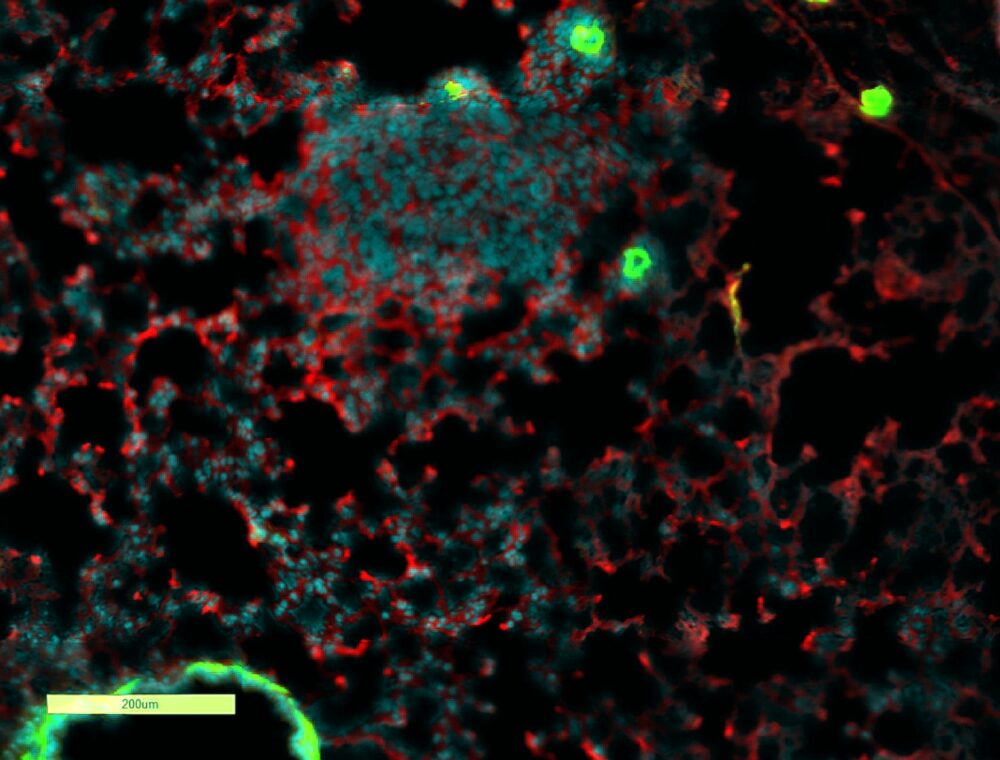
What exactly is going on in the lungs?
Fibroblasts – cells found in connective tissues – become activated and inflamed by chemotherapy-induced tissue damage. The fibroblasts then secrete proteins that prompt immune cells to travel from the bone marrow to the lungs.
“In this way, the chemotherapy administered as a means for combating cancer achieves the opposite result,” Erez says.
Opening the black box
The researchers identified the mechanism through which fibroblasts recruit immune cells – a process called chemotaxis – and “train” them to support the cancer.
Once the researchers had identified the offending proteins, an existing drug known to block the activity of so-called “complement proteins” to cause inflammation was added to the mouse mix.
The researchers didn’t know if this inflammation inhibitor would prevent a relapse, but it did.
The treatment combination resulted in the percentage of animals developing no metastases at all rising from 32% to 67%. The percentage of animals with extensive cancer colonization in their lungs was reduced from 52% to 6%.
The mice that received the new treatment went through the same process as a human patient with breast cancer: surgical removal of the primary tumor, then chemotherapy, followed by monitoring to detect metastatic relapse as early as possible.
The animals’ lungs were examined at an intermediate stage – when tiny micro-metastases may have already developed but even advanced imaging technologies like CT scanning cannot find them.
Erez calls this interval between chemo and detection “an inaccessible ‘black box.’ Working with an animal model, we could check what actually happens inside this ‘box.’”
The study was led by Erez of the department of pathology at TAU’s Sackler Faculty of Medicine, and researchers from her group: Lea Monteran, Dr. Nour Ershaid, Yael Zait, and Ye’ela Scharff, in collaboration with Prof. Iris Barshack of the Sheba Medical Center and Dr. Amir Sonnenblick of the Tel Aviv Sourasky Medical Center. The study was funded by ERC, the Israel Cancer Association, and the Emerson Collective Cancer Research Fund.
“We hope that our findings will enable more effective treatment for breast cancer, and perhaps other types of cancer as well – to prevent metastatic relapse and save numerous lives worldwide,” Erez says.