A diagnostic system developed at the Technion-Israel Institute of Technology enables rapid and accurate customization of an antibiotic to a patient.
If the system is commercialized, patients with life-threatening infections or in need of urgent treatment will enjoy faster diagnostics, earlier and more effective treatment of infectious bacteria and improved recovery times.
The findings related to the new Technion diagnostic system were published recently in the Proceedings of the National Academy of Sciences (PNAS).
Antibiotics are one of the most effective ways to treat bacterial infections. But widespread use of antibiotics accelerates the development of resistant bacterial strains.
In fact, in June, the World Health Organization updated its Essential Medicines List with new advice on use of antibiotics.
“The rise in antibiotic resistance stems from how we are using – and misusing – these medicines,” said Dr Suzanne Hill, director of Essential Medicines and Health Products. “The new WHO list should help health system planners and prescribers ensure people who need antibiotics have access to them, and ensure they get the right one, so that the problem of resistance doesn’t get worse.”
In 2014, infections with antimicrobial resistance (AMR) claimed the lives of more than 700,000 people worldwide, in addition to a cumulative expenditure of $35 billion a year in the US alone, reports the Technion.
According to established estimates, for every hour that effective antibiotic treatment is delayed, survival rates drop by about 7.6% for patients with septic shock. Therefore, in order not to leave the patient without adequate protection while awaiting the results, many doctors will prescribe an antibiotic with a broad spectrum of activity in large doses. This phenomenon facilitates the emergence of AMR and also affects the microbiota – the population of “good bacteria” found in the human body that protects it.
“Every day, tens to hundreds of tests are carried out at every hospital in Israel to map the resistance levels of infectious bacteria from samples taken from patients. The problem is that this is a very long test, since it is based on sending the sample to the lab, growing a bacterial culture in a petri dish and analyzing the culture. This process requires relatively large sampling and usually takes a few days, in part because the workday at labs is limited to around eight hours,” said Technion doctoral student Jonathan Avesar, one of the researchers on the new system.
“Our method, on the other hand, provides accurate results in a short time based on a much smaller sample. It is obvious that a faster response allows us to start treatment earlier and improve the speed of recovery.”
Fast results
The innovative system developed at the Technion, called the SNDA-AST, quickly analyzes bacteria isolated from patients with infections and assesses their level of resistance to specific antibiotics. This enables the healthcare team to choose the most effective antibiotic a day earlier than when using traditional methods.
Technion researchers demonstrated the ability to test bacteria directly from patient urine samples, thus skipping the isolation step and potentially saving two days for patients with urinary-tract infections.
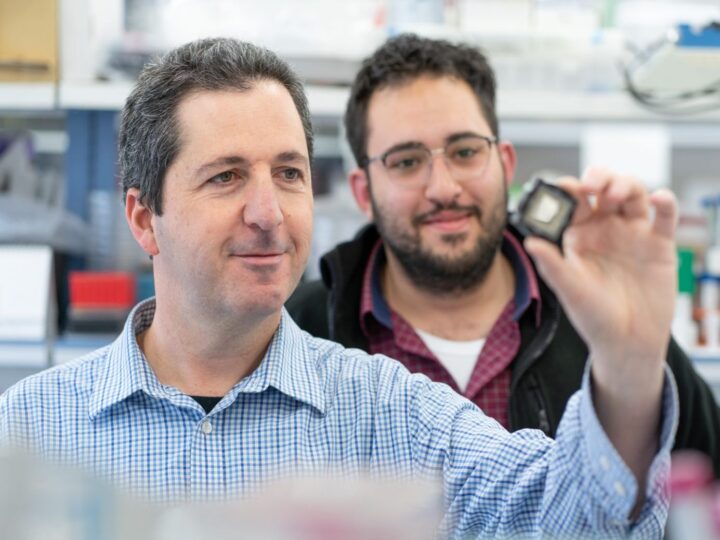
They developed a chip with hundreds of nanoliter (1,000 times smaller than a milliliter) wells inside it, each containing a few bacteria and a specific antibiotic. Detection of the bacterial response is done using a fluorescent marker, image-processing tools and statistical analysis of the colors obtained from the bacteria in all the nanoliter wells.
The study tested 12 bacteria-antibiotic combinations.
“The use of the technology that we developed reduces the size of the required sample by several orders of magnitude, reduces the scanning time by around 50%, significantly reduces the lab space required for testing and reduces the cost per test,” said Avesar.
The study was led by Prof. Shulamit Levenberg, dean of the Technion Faculty of Biomedical Engineering, and was carried out in her lab by Avesar, postdoctoral student Dekel Rosenfeld and doctoral student Tom Ben-Arye.
Also contributing were Assistant Prof. Moran Bercovici of the Technion Faculty of Mechanical Engineering, doctoral student Marianna Truman-Rosentsvit and Dr. Yuval Geffen, head of the Microbiology Laboratory at Rambam Health Care Campus in Haifa. The study was funded by a KAMIN grant from the Israel Innovation Authority and the Israeli Centers of Research Excellence (I-CORE).