For Prof. Beka Solomon it was obvious. If it isn’t possible to send drugs to the brain to treat Alzheimer’s disease the normal way because of the blood-brain barrier that prevents drugs from moving from the blood stream into the brain, then send them through the nose instead.
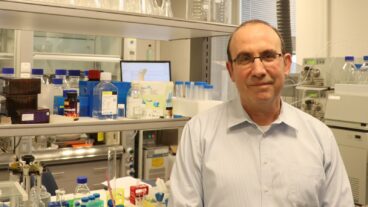
Solomon, of the Molecular Microbiology and Biotechnology Department at Tel Aviv University, has been working in this field for the last 13 years after years of research in immunotherapy, and found in mouse trials that filamentous phages, a harmless bacterial virus found almost everywhere from the depths of the ocean to the lining of the stomach, can be an effective treatment against Alzheimer’s disease when carried to the brain through the nose.
Alzheimer’s is a debilitating disease that leads to progressive loss of memory and cognitive functions, and a great deal of suffering for both the person afflicted and their loved ones. In the US alone, there are now more than five million people living with Alzheimer’s, but there is currently no drug on the market that can cure or effectively stop the progression of this disease.
The cause of this disease and other neurological diseases like amyotrophic lateral sclerosis (ALS) is widely concluded to be plaque formation, which causes inflammation in the brain. Up to now, scientists working on a cure for the disease have focused on dissolving and preventing plaque formation, but most have come up against two problems ? firstly the difficulty in developing drugs that pass through the highly selective blood-brain barrier; and secondly unwanted side-effects of inflammation and hemorrhaging.
In her research Solomon shows that by administering non-lytic filamentous phages in small doses through the nasal passages, the phages have a direct and rapid route to the brain. There they lock onto the extracellular plaques associated with Alzheimer’s and dissolve them, reducing inflammation in the brain without any side effects. The body then gets rid of the waste naturally.
“The filamentous phages have a nanotubular appearance which is very similar in shape to amyloid fibrils, the main component of amyloid plaque, which is the plaque linked to Alzheimer’s,” explains Solomon, who recently presented her findings at a meeting of the American Society for Microbiology in Canada.
Solomon first began thinking about sending phages through the nasal passages because the plaque that causes Alzheimer’s first appears in the olfactory bulb. As a result, one of the early symptoms of this devastating disease is loss of smell.
To test her hypothesis, Solomon and her colleagues treated 150 mice with the phage internasally for 12 months. They found the mice that had exhibited the symptoms of Alzheimer’s regained their sense of smell and also showed memory and cognitive improvement. After one year of treatment, they had 80 percent fewer plaques than untreated mice.
The phages were eliminated from the brain and secreted from the body in urine and feces. The researchers saw no adverse effects in the peripheral organs – the kidneys, liver, lungs, and spleen biology were all normal.
“The mice showed very nice recovery of their cognitive function,” says Solomon, who emigrated with her family to Israel from Romania about 40 years ago. “We saw a reduction in the ameloid plaque and a reduction in brain inflammation. Afterward the phages were eliminated naturally from the body through the kidneys without any adverse side-effects.”
“This is a potential breakthrough, but it needs to be proved further,” Solomon told ISRAEL21c. “Bateriophages are one of the most numerous life forms on earth and mammalian organisms are very frequently exposed to interactions with them. We know for instance that they are a very important part of the natural flora of the gut and research groups all over the world have developed classic phage therapy as an alternative to antibiotics. We are used to living with them, it’s not unusual, but to take them to the brain in unusual. This is the first attempt to use phages as a treatment for Alzheimer’s.”
Ramot, the commercial arm of Tel Aviv University is now planning to commercialize Solomon’s research and has licensed the technology to a startup company.
“Beka is a real pioneer in developing an immunotherapeutic approach for the treatment of Alzheimer’s disease,” says Irit Ben-Chlouch, director of business development, life sciences at Ramot. “She was the first to show the disease can be treated using antibodies and, as the main focus of her lab, has developed several different breakthrough approaches.”
In the meantime, Solomon plans to continue with her research, which she regards as a platform technology. She and fellow researchers at the university are now exploring whether this intranasal administration of filamentous phages can also be used to help patients suffering from Parkinson’s disease and Huntingdon’s disease.
She is also exploring the possibility of adding medicines, such as anti-inflammation agents to the phages, to bring the brain additional therapeutic medicines. ![]()