‘Our study showed that there was an inverse relationship between the amount of antibodies in children in a community and the incidence of the disease.” – Prof. Justen Passwell. An Israeli research team is leading a clinical study which could lead to stamping out shigella, one of the world’s most deadly diseases and the killer of an estimated one million children each year.
Shigella dysentery is a common disease, often self-limited and mild but occasionally serious, particularly in the first 3 years of life. Poor sanitary conditions promote the spread of shigella. Shigella is transmitted primarily from person-to-person by the fecal-oral route, which has been known to occur in day-care centers. Occasionally, outbreaks can be caused by contamination of food by infected food handlers.
WHO officials have designated finding a vaccine for this bacterial disease to be a top international health priority, but until now have been frustrated in their attempts to develop one. One complicating factor has been testing potential treatments on shigella-affected populations which are mainly located in the developing world. To do so means having close proximity to the sophisticated on-site medical staff and laboratory systems needed to support clinical trials.
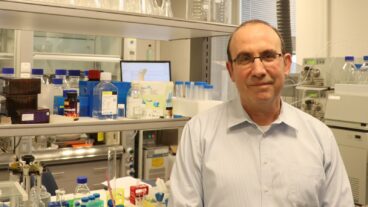
Enter Prof. Justen Passwell, the Director of Pediatrics at the Sheba Medical Center in Tel Hashomer. Passwell was aware that among Israel’s heterogeneous population there were communities where outbreaks of shigella occurred and had himself about ten years ago gained international recognition for spotting an occurrence of a rare form. He also was personally familiar with the groundbreaking work carried out by Dr. Rachel Schneerson and Dr. John Robbins of the US National Institute of Health in developing conjugate vaccines.
It was the introduction of a conjugate vaccine developed by Schneerson and Robbins for another bacterial disease – bacterial meningitis – that effectively eliminated the disease. This effort also established an important scientific principle: that when the polysaccharide of a bacteria is bound to another protein it elicits an immune response in young toddlers that enables them to be protective of a bacterial disease.
“We did a preliminary study to look at the antibodies of shigella and showed that there was an inverse relationship between the amount of antibodies in children in a community and the incidence of the disease. This gave us the rationale for suggesting that developing the right kind of conjugate vaccine could prevent outbreaks of shigella,” says Passwell.
In 1997 the NIH decided to provide major funding for a multi-stage clinical trial program in Israel headed by Passwell. Since then the Israel Shigella Group has conducted three safety and immunogenicity studies, many of them especially complicated both in design and implementation. Five different vaccines were tested in adults involving different combinations of protein carriers and succinylation of protein carriers prior to the selection of a lead compound.
These studies were particularly difficult in the toddlers, the most susceptible age group, because of the frequent blood samples required to document the required immunogenicity following immunization. All experimental procedures have been done with FDA approval.
“Testing a vaccine in a small pilot group is especially difficult because you don’t know when and in what part of the country an outbreak will occur,” observes Passwell. To meet this challenge, peripheral sites at various locations in the country were established for recruitment of volunteers and monitoring after the immunization. To facilitate the monitoring the Israeli Shigella Group developed a computerized database and with the collaboration of one of the the major Israeli HMOs, the collection of stool samples enabling the monitoring of the incidence of Shigellosis among the immunized toddlers in various geographic regions has been possible.
Passwell points out that the first safety and immunogenicity studies have been successfully concluded and a major efficacy study among young children, aimed at corroborating findings made in adult studies is now underway. If all goes as planned the clinical testing program will be completed in about two years, setting the stage for a mass inoculation program in the developing world.
To do so, Passwell emphasizes, a commercial manufacturer will have to come forward and implement a program of this kind, but the scientific work will be complete and the dream of stamping out shigella and saving an enormous number of lives will be within reach.
The NIH-Israel Shigella Group collaboration already serves as an inspiration for researchers around the world. At a time when the bio-medical industry is being criticized for focusing on developing health products for the benefit of consumers in the developed world, the Shigella project shows how the scientific community can be harnessed to serve some of the world`s neediest people.
(Reprinted from BioIsrael)